
Weight Loss Drugs
GLP-1 Peptides: Weighing the Risks, Benefits, Costs, and Ethical Implications
“Assess the prevalence of and threat posed by the prescription of…weight-loss drugs”
GLP-1 receptor agonists and dual GLP-1–GIP receptor agonists (hereafter referred to as “GLP1s”) have been described as a revolution in obesity and type 2 diabetes management. These peptides, including semaglutide and tirzepatide, mimic elevated GLP1 to supraphysiologic levels to regulate blood sugar levels and appetite. However, like any medical intervention, there are limitations and risks.
As the nation tackles the obesity epidemic now affecting over a 1/3 of the U.S. population and its widespread impact— including the high cost of public prevention, the unsustainable expense of medical treatment, and the physical and economic burden of the disease— we must explore effective and cost-effective therapies and treatment optimization.
The unfortunate “necessity” of these medications is discussed in other sections of this report. In public health, we all recognize that prevention is more effective than treatment. Unfortunately, a significant portion of the population requires intensive intervention. Many patients with obesity and/or prediabetes go undiagnosed and untreated leading to disease progression. GLP1 use will continue to grow as their approved indications expand, drugs become more effective, and ideally, costs will eventually align with global standards. However, risks and limitations have emerged.
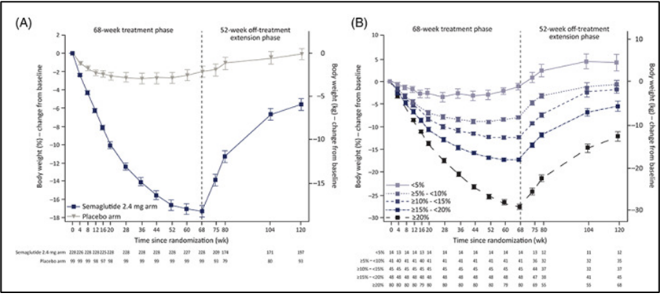
Pharmaceutical and medical claim records indicate that 68% of patients discontinue GLP1 drug classes within 1 year of initiating. Most notably, upon medication cessation, weight regain is rapid leading many public health officials to argue that patients must remain on them indefinitely marking an unsustainable public health dilemma.
Drug cost can often exceed >$12,000/year with analyses from the Institute for Clinical Economics Review demonstrating that GLP1 drugs cost two-fold higher than their expected value from weight-loss-associated reductions in cardiovascular events and diabetes lifestyle management. Historically, major supplies (Eli Lilly and Novo Nordisk) cannot match healthcare demands, limiting access. 30-50% of people with diabetes report anxiety and/or fear of injections, which may be even higher in the general public who are unfamiliar with continuous syringe or needle treatments. There are also several known acute and chronic side effects of GLP1a administration.
Potential Risks (not all-inclusive):
- Common gastrointestinal side effects: nausea, vomiting, diarrhea (30-50% of users) [1] [2]
- Potential loss of lean mass (25-40%) [3
- Rare but serious risk of acute pancreatitis [4] [5]
- Increased risk of gallbladder disease, including gallstones [6]
- Potential for acute kidney injury, especially due to dehydration from GI side effects [7] [8]
- Possible increased risk of thyroid cancer (though human data remain inconclusive) [9]
- Risk of hypoglycemia when combined with insulin or sulfonylureas [10]
- High cost and discontinuation rate [11]
However, as GLP1 only works so long as they are continually administered, some speculate that life-long administration may be required and the long-term effect of these drugs beyond 5 years remains largely unknown. While inherent limitations are revolving these limitations require alternative cost-effective lifestyle treatments, this document provides a fundamental overview of the benefits, risks, and costs of the medication. More importantly, it offers a framework for clinicians to assess appropriate use and optimize treatment. Our discussion will be guided by the Four Pillars of Medical Ethics, which safeguard patients from harm while enabling physicians to follow their conscience and exercise professional judgment. Any conversation about these medications must be intertwined with the principles of medical ethics.
1st Pillar of Medical Ethics: Autonomy
Patient self-determination is a fundamental principle in medical treatment, encompassing informed consent, confidentiality, truth-telling, and protection against coercion. Genuine informed consent is an ongoing process that requires a competent patient, full disclosure of the proposed treatment, clear understanding, and voluntary agreement. When it comes to GLP1s, true informed consent must include a thorough discussion of its potential benefits, known and unknown risks, and the necessary support and behavior changes for optimal use. Only through this approach can we ensure the effective medical and financial use of this medication on a national scale. Over the past decade, countless articles have explored the growing list of medical indications and potential benefits of these highly sought-after medications, alongside their associated risks [12] [13] [14] [15] [16] [17] [18] [19] [20] [21].
2nd Pillar of Medical Ethics: Beneficence
The second pillar of medical ethics, Beneficence, requires physicians to act in the best interests of their patients. Every treatment or procedure should provide a clear benefit to the individual receiving it. If a procedure offers no advantage to a patient, it should not be performed. Ethical medical practice prioritizes personal well-being over collective interests.
GLP1 Potential Benefits (not all inclusive):
- Significant weight loss (10-20% in obese patients at over a year) [22] [23] [24]
- Improved glycemic control in type 2 diabetes [25] [26]
- Reduced risk of major adverse cardiovascular events [27] [28]
- Improved kidney function and slowed progression of diabetic kidney disease [29] [30]
- Potential neuroprotective effects for conditions like Alzheimer’s and Parkinson’s [31] [32]
- Reduced addiction to substances like alcohol and substance use [33] [34] [35]
- Reduced visceral fat and liver fat [36] [37]
- Improved musculoskeletal health [38] [39]
It is also essential to lay out alternative treatment paths. Most notably, low or no-cost nutritional intervention.
Low-carbohydrate or ketogenic diet benefits (not all inclusive):
- * Significant weight loss (10-20% over a year)
- Weight loss is greater with low-carbohydrate and ketogenic diets (10-15%) in type 2 diabetes than current GLP1 (5%) [40] [41]
- Type 2 diabetes remission in >50% of patient (<5.7% HbA1c without medication) [42] [43] [44]
- Reduced metabolic-associated steatotic liver disease (previously known as Non-Alcoholic Fatty Liver Disease).[45] [46]
- Deprescription and annualized healthcare cost savings $5000/patient to >$10,000/patient.
- Demonstrated ability to off-ramp GLP1a [47] [48]
- Juvenile diabetes (<5.7% HbA1c with only medicinal insulin) [49] [50] [51]
- Rapid reversal of prediabetes (<4 weeks) [52] [53]
- Seizure reduction in drug-resistance epilepsy [54] (~10% of patients with epilepsy are cured after diet cessation [55])
- Improved cognition and mental state in Alzheimer’s [56] and age-related cognitive decline [57]
- Potential ability to improve kidney disease [58]
3rd Pillar of Medical Ethics – Non-Maleficence
The third pillar of medical ethics, Non-Maleficence, is rooted in the principle primum non nocere—“First, do no harm.” Any treatment or procedure with a higher risk of harm than benefit should not be performed. Ethical medicine demands careful risk-benefit assessment (see risk above) to protect patient well-being and consideration for alternative treatment paths (see low carbohydrate diet above).
4th Pillar of Medical Ethics – Justice
Justice—the ethical imperative to distribute limited healthcare resources fairly—is especially relevant as the use of costly GLP-1 medications has surged for obesity even as their use for diabetes declines, creating stark disparities in access between higher- and lower-income patients. With U.S. prices far exceeding those abroad and Senate projections estimating up to $1 trillion in annual prescription spending (and $411 billion if broadly used for obesity [59]), programs like Medicare and Medicaid face unsustainable strain that threatens access for those most at risk. Ethically, clinicians must balance promoting these effective treatments against financial constraints by prioritizing patients who will gain the most “potential years of life lost” (PYLL) benefit—particularly younger, severely affected individuals—and focus on prevention of type 2 diabetes. As Emanuel argued in NEJM [60], and Dellgren and colleagues reiterated in The Lancet [61] and Annals of Internal Medicine [62], blanket coverage denials are unjust; instead, targeted coverage for those with the strongest claims aligns with both cost-effectiveness and justice until policy, supply, and pricing reforms ensure equitable access.
Conclusion: Balancing Risks, Benefits, and Costs
GLP-1 receptor agonists have ushered in a revolutionary era in obesity and type 2 diabetes care—offering dramatic weight loss, improved glycemic control, and meaningful reductions in cardiovascular and renal risk—but their extraordinary benefits are tempered by significant side effects, high discontinuation rates, lifelong dependency, and annual price tags exceeding $12,000/patient and $1 trillion in annual prescription spending that threaten both individual patients and the sustainability of our healthcare system. As lifestyle is frontline therapy, low carbohydrate and ketogenic eating strategies are underutilized therapeutic strategies shown to be safe, and induce profound weight loss, diabetes remission, MASLD reversal, and neurological protection while saving $5000 to >$10,000 in healthcare costs per patient. GLP1 administration must be anchored in the four pillars of medical ethics—that maximizes benefit, minimizes harm, and ensures equitable care for the most vulnerable.
Dr. Mark Cucuzzella, a family physician and professor at West Virginia University School of Medicine speaks nationally on judicious approach to GLP-1 medications, advocating for their targeted use in high-risk patients while emphasizing lifestyle interventions and nutritional therapies to address the root causes of metabolic disorders
Andrew Koutnik, PhD, is an award‑winning Research Scientist and globally recognized authority on metabolic health, diabetes management, and human performance optimization, having collaborated with leading institutions such as NASA, John Hopkins, Harvard Medical School, and the Department of Defense, amongst others. Dr. Koutnik was diagnosed with Obesity and Juvenile Diabetes in adolescence and has investigated lifestyle intervention to prevent and eliminate chronic disease burden.
Appendix:
Comprehensive Video from the author: Once and Future Use of GLP1 In the Framework of The Four Pillars Of Medical Ethics
Download slides in the note section. Video is unlisted https://www.youtube.com/watch?v=41Ptth0lEnU
Article Reference: Weight Loss Drugs – References





