
Corporate America
Proposal to Expand Access to Effective Metabolic Health Care in Corporate America.
Defining the Problem: The Human and Financial Cost of Metabolic Disease
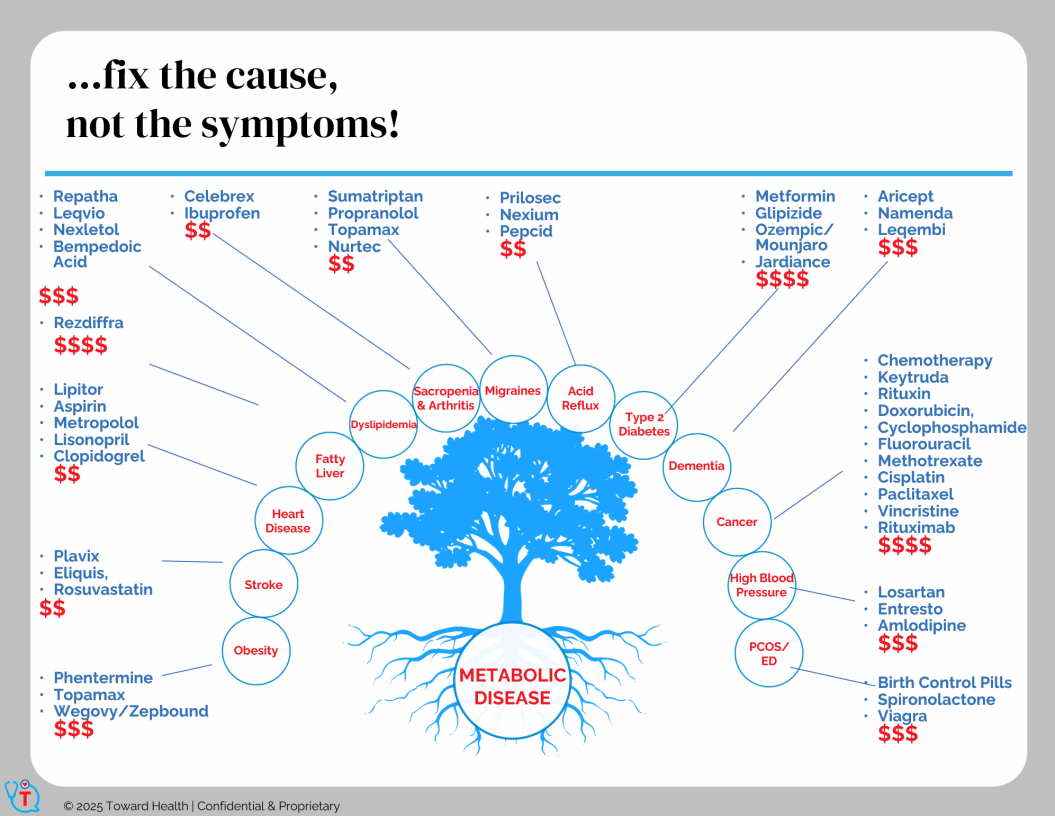
Metabolic diseases—including diabetes, hypertension, and heart disease—are leading causes of disability, loss of life, and rising healthcare costs in the U.S. Current management focuses on symptom control rather than addressing root causes, leaving patients dependent on costly medications and recurring treatments. The toll extends beyond personal suffering, costing billions in direct medical expenses and lost productivity.
Defining the Problem for Corporate America
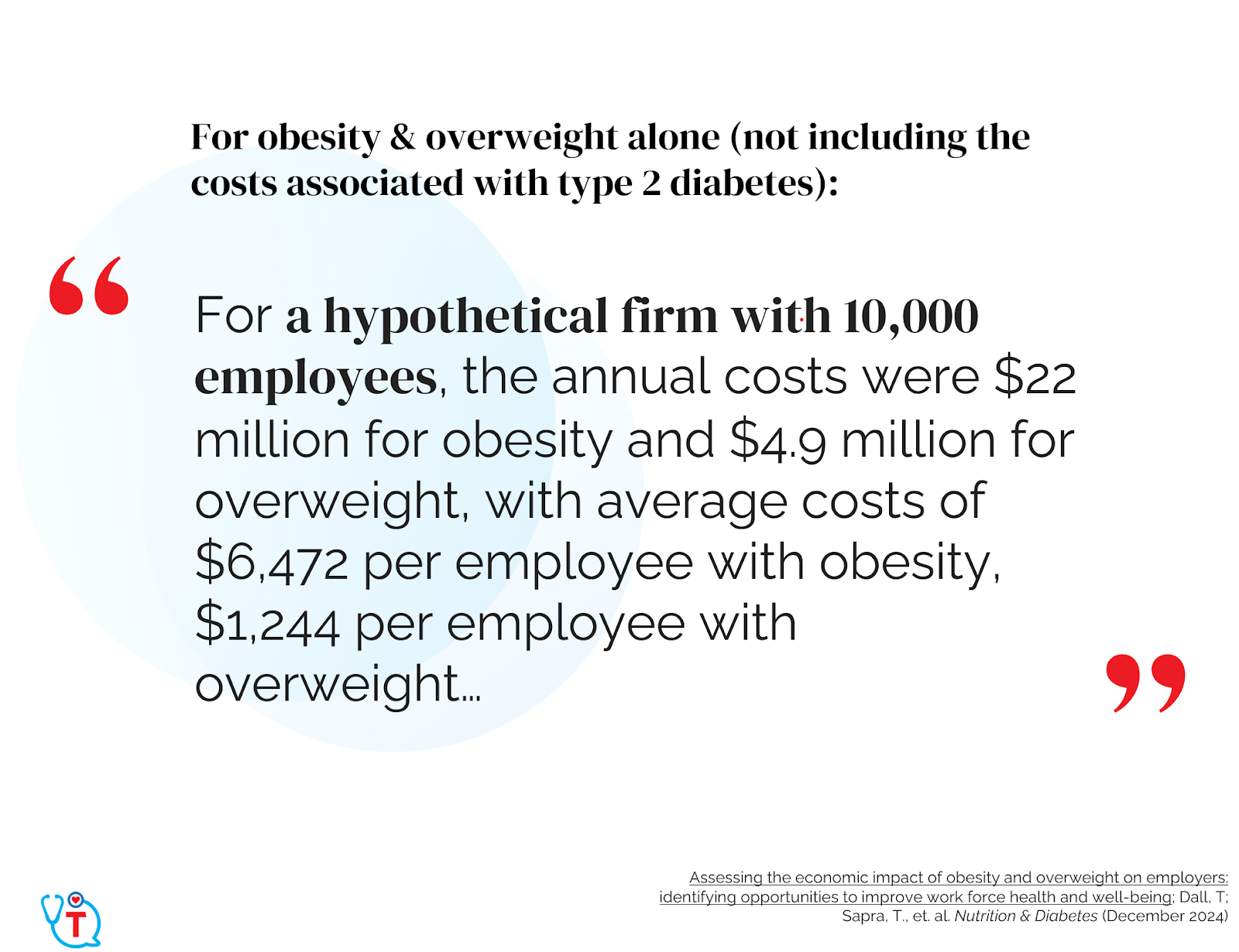
Healthcare costs and productivity losses for employers have increased by 170% since 2000, adjusted for inflation. Metabolic Syndrome, identified by obesity, high blood pressure, high blood sugar, high triglycerides or low HDL cholesterol, is debilitating our employee base and driving a substantial part of the cost increase.
The average additional annual cost for healthcare and lost productivity for an employee with obesity and type 2 diabetes versus a healthy employee is ~$20,000 (not including GLP-1 medications).
https://pmc.ncbi.nlm.nih.gov/articles/PMC11618327
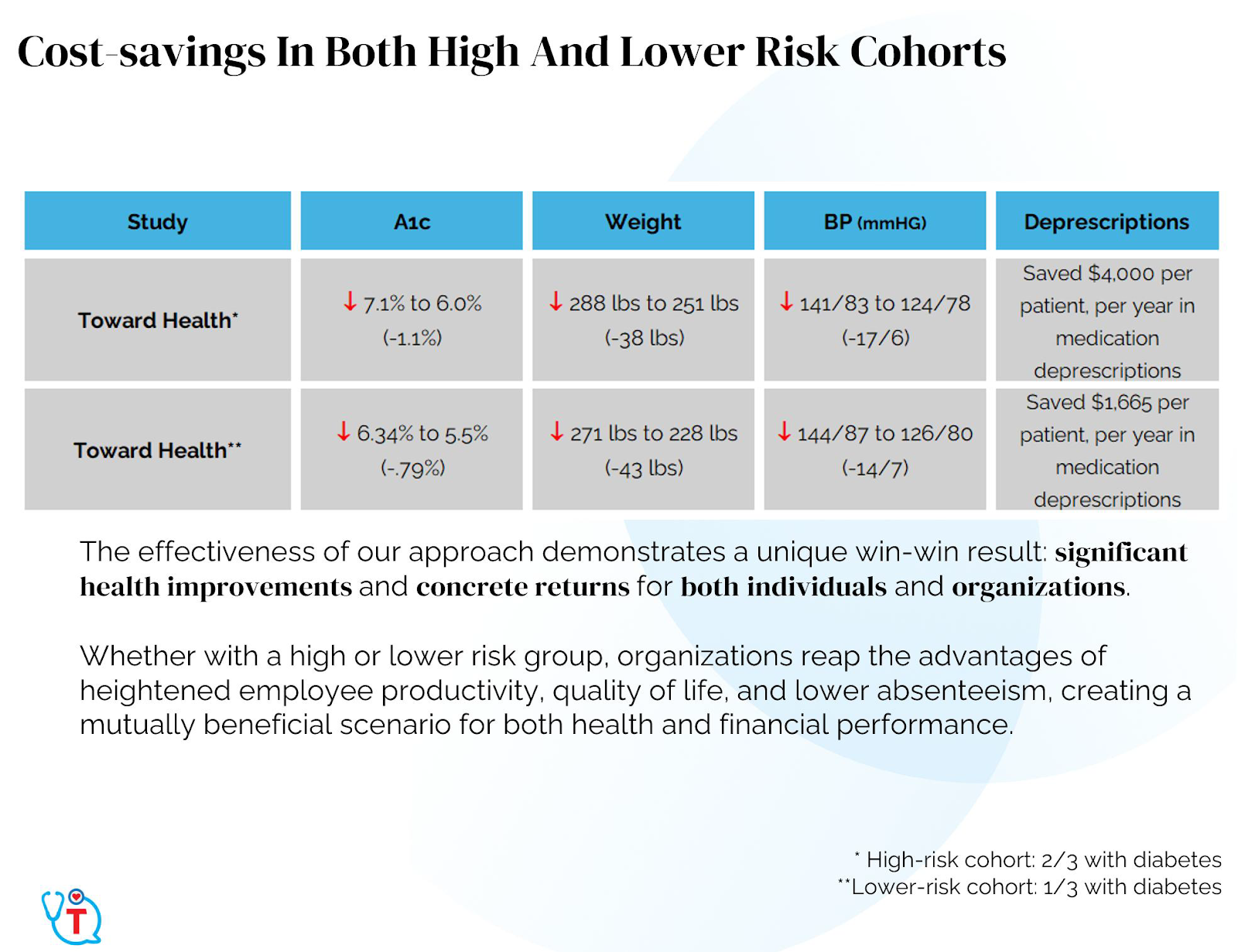
Real-World Interventions Using Metabolic Dietary Approaches
Practices like Virta Health, Dr. David Unwin’s clinic, and Dr. Tro Kalayjian’s practice (Toward Health) have demonstrated that technology and reducing carbohydrate intake and targeting metabolic health directly can yield significant improvements in patient outcomes, reducing medication needs and associated costs. These models provide compelling evidence for dietary-based, multi-modal care in managing and reversing metabolic diseases. Disease remission is a well-documented and long term possibility through these programs and other similar programs that focus on lifestyle, low-carbohydrate diets as well as remote monitoring and other technological innovations.

https://pmc.ncbi.nlm.nih.gov/articles/PMC11868080/
https://pmc.ncbi.nlm.nih.gov/articles/PMC9505533/
The Financial Risks of Current Medication-Dependent Approaches
Current strategies for managing diabetes and metabolic diseases, heavily reliant on high-cost medications like GLP-1 and SGLT2 inhibitors, address symptoms rather than underlying causes. At $1,000 per month per patient and with generics not expected until 2040, this medication-dependent approach risks bankrupting the healthcare system. Multi-modal practices that utilize remote monitoring nationwide and leverage metabolic dietary approaches present a more sustainable solution, reducing costs while enhancing outcomes.
Corporate America is the Ideal Partner
Corporate America is the ideal partner to promote health because they will see the direct financial reward from creating a happy and healthy workforce. By increasing employee happiness, metabolic health and lowering their burden of chronic disease the employer can reap the rewards of a more productive workforce that has decreased drug and medical cost. Corporate America cannot continue to subsidize the mental and metabolic health cost burden from our modern processed food.
Reducing Regulatory Barriers to Deliver Nationwide Metabolic Health Care
To deliver effective, multi-disciplinary care across the country, practices like ours need licensed professionals—NPs, PAs, mental health counselors, and physicians—approved in all 50 states, each with unique regulatory demands. This level of regulatory complexity makes it nearly impossible to scale care nationwide. Streamlining these requirements would enable broader access to high-quality, affordable care, ultimately addressing the growing metabolic health crisis more effectively and efficiently.
Addressing Regulatory Barriers to Technology and Investment in Physician Practices
Current regulations restrict physician practices from accepting external investments in many states, blocking access to capital that could fund essential technology upgrades and interoperability. These barriers prevent practices from adopting advanced tools and integrated systems that would enhance patient care and outcomes. Allowing responsible outside investment, with appropriate safeguards, would empower physicians to modernize their practices, improve efficiency, and meet the rising demand for quality care in metabolic health.
Proposed Solutions and Requests for Federal Support
- Subsidize Corporate Metabolic Health Programs
- Provide subsidies or tax credits for corporations investing in employee health and provide incentives for reducing chronic disease in their workforce.
- Reduce Costs for Nationwide Telehealth in Metabolic Practices
- Remove regulations that limit nationwide metabolic telemedicine practices to meet the demands of our chronic disease epidemic.
- CMS Reimbursement for Direct Primary Care providers
- Update CMS policies to support reimbursement for Direct Primary Care, reducing physician burnout and allow CMS to evaluate the cost-effectiveness of multi-modal approaches that reduce dependence on costly medication, focusing on long-term health outcomes and savings.
- Adequate Reimbursement to Recruit and Sustain Metabolic Health Providers
- Adjust reimbursement rates to attract and sustain a robust workforce of metabolic health specialists, enabling widespread implementation of diabetes reversal programs.
- Streamline Multi-State Licensing for Nationwide Telehealth
- Implement a federal telehealth licensing standard, allowing metabolic health providers to practice across state lines without redundant requirements, including mental health counselors, psychiatrists, physicians, physical therapist, Pas, and NPs.
- Enable Outside Investments in Physician Practices for Technology Modernization
- Allow regulated external investments in physician practices to support critical technology upgrades and interoperability, fostering a modern, efficient healthcare system.
- Introduce Federal Incentives for Interoperable Technology
- Offer grants or tax incentives for practices implementing interoperable health technologies, boosting care coordination and remote monitoring capabilities for metabolic disease.
- NIH Funding for Independent, Root-Cause Focused Research
- Provide NIH grants for independent research into dietary and lifestyle interventions, free from corporate interests, to advance evidence-based, root-cause treatments for metabolic disease.
- Create Diabetes Reversal Centers of Excellence
- Establish and fund regional centers dedicated to diabetes reversal, targeting high-need areas and using proven models to drive effective and equitable care.
Dr. Tro Kalayjian, a board-certified physician in Internal Medicine and Obesity Medicine, transformed his own health by losing 150 pounds and now leads a pioneering medical practice that has helped patients collectively lose nearly 100,000 pounds through personalized, evidence-based metabolic intervention.
Article Reference: Corporate America – References





