
South Bronx
Tackling Diabetes in the Bronx – The Epicenter of the Diabetes Epidemic
INTRODUCTION
The Bronx represents a microcosm of America’s metabolic health crisis, with rates of type 2 diabetes, obesity, and related disorders substantially exceeding national averages and disproportionately affecting low-income populations. This metabolic disease burden stems from systemic issues including food access inequities, economic constraints, and misguided nutritional guidance. While conventional “eat less, move more” approaches have failed to reverse these trends, emerging evidence demonstrates that therapeutic nutritional interventions targeting carbohydrate reduction can achieve rapid metabolic improvements and functional remission of disease. The Bronx Project represents an opportunity to implement evidence-based nutritional approaches at the community level, potentially transforming one of America’s most metabolically challenged communities into a model for nationwide intervention.
INCIDENCE: The Metabolic Health Crisis in the Bronx
The Bronx exhibits one of the nation’s highest diabetes rates estimated between 13.5% and 18% 1,2,3, which is considerably higher than the national prevalence of 8.9%.4 Particularly alarming is the trajectory, as a Montefiore institute study showed diabetes prevalence in the Bronx jumped from about 12% in 2002 to 17.5% by 2017, a near 50% increase (See Figure 1).3 When considering that over 37% of adults are obese 5 and poverty rates exceed 27%6, the highest amongst any NYC county,7 estimates suggest an additional 7% of the Bronx may have undiagnosed diabetes.8,9,10
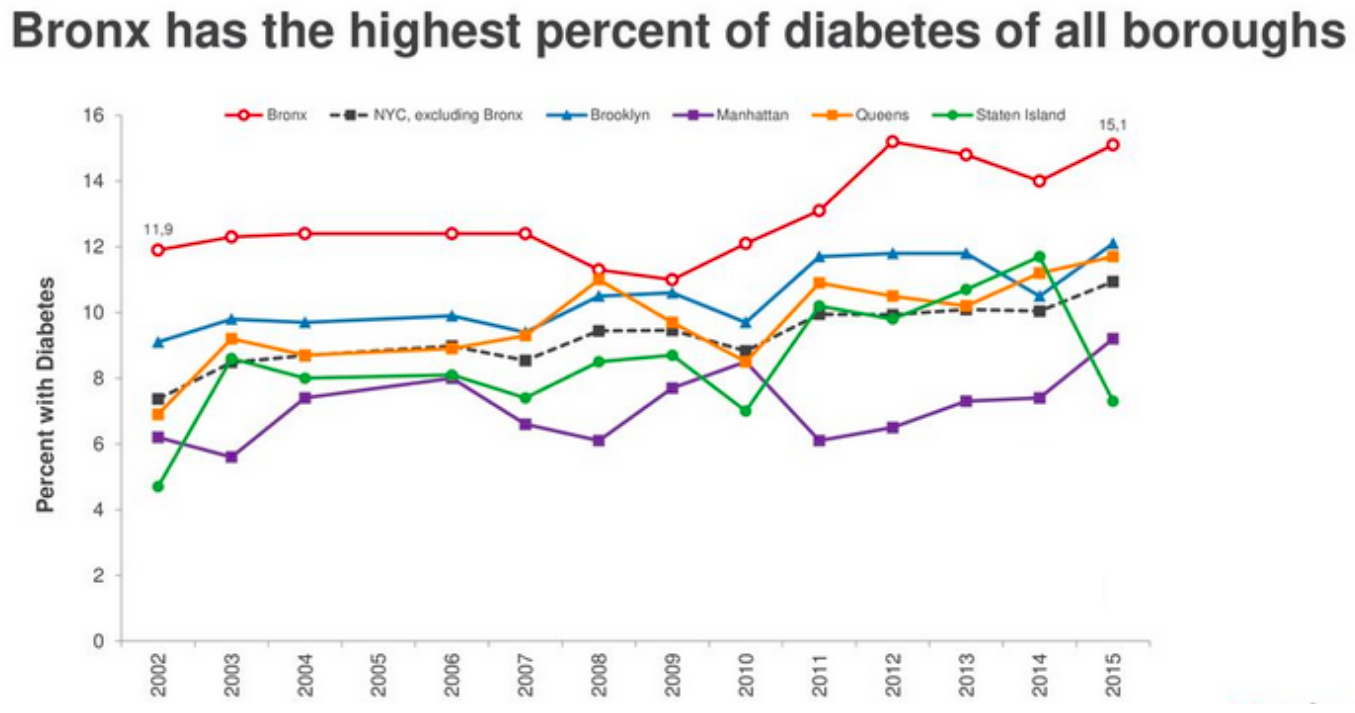
Figure 1: Diabetes prevalence across NYC boroughs from 2002 – 20153
ROOT CAUSES: Environmental Factors
Studies suggest that the metabolic crisis amongst minorities may stem primarily from environmental and socioeconomic factors, rather than genetics.11 While many elements contribute to this crisis, food environment and dietary patterns represent the most immediately modifiable factors.12,13
The traditional diets of many Bronx communities—including rice and beans, plantains and tubers in Caribbean, Latin American and African cuisines—have historically been balanced with whole foods.14 However, these carbohydrate components now comprise an outsized portion of meals, while being combined with modern additions like refined sugar and industrial seed oils. NYC Department of Health data shows that residents in the South Bronx consume sugar-sweetened beverages at rates 42% higher than the city average.15 Furthermore, according to USDA Economic Research Service data, households in the lowest income quartile spend 35% less time cooking at home compared to higher-income households, leading to greater reliance on prepared and ultra-processed foods.16
The Bronx also contains numerous “food swamps” where 72% of food retailers primarily sell ultra-processed, high-carbohydrate options, while fresh, unprocessed foods are scarce.17 Further aggravating the issue, research indicates that predatory marketing takes place in New York where its low-income communities can receive almost double the amount of food and beverage marketing compared to its high-income communities.18,19
Biological Impact: Insulin Resistance
Insulin resistance represents the core pathophysiological defect underlying type 2 diabetes.
Chronic carbohydrate/sugar overconsumption necessitates repeated insulin secretion, as insulin is the primary hormone responsible for glucose clearance from the bloodstream. The more frequent and the higher insulin spikes, the more it leads to a downregulation of insulin receptors, and hence less glucose uptake. This becomes a positive feedback cycle, whereby now the pancreatic β-cells must compensate for this decrease in glucose uptake by secreting higher insulin levels to maintain euglycemia.20
This compensatory hyperinsulinemia triggers a cascade of cellular adaptations. The insulin receptor substrate-1 (IRS-1) undergoes serine phosphorylation rather than tyrosine phosphorylation, inhibiting the insulin signaling pathway. Concomitantly, inflammatory mediators such as tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) increase, further impairing insulin signaling. The phosphoinositide 3-kinase (PI3K) pathway becomes progressively impaired, reducing glucose transporter type 4 (GLUT4) translocation to cell membranes and diminishing glucose uptake in skeletal muscle and adipose tissue.21 As insulin resistance progresses, hepatic glucose production becomes dysregulated, with failure of insulin to suppress gluconeogenesis.22 Adipocyte dysfunction leads to increased free fatty acid release, which further exacerbates insulin resistance through lipotoxicity.23 In many people, eventually pancreatic β-cell function deteriorates due to glucotoxicity, lipotoxicity, and amyloid deposition, leading to insulin deficiency relative to the amount of insulin needed to overcome the insulin resistance, and type 2 diabetes sets in.24
Diabetes is only one of the many manifestations of insulin resistance. Insulin resistance can present as high blood pressure,obesity, and atherogenic dyslipidemia.25 It can also present as CVD,26 Alzheimer’s disease (AD),27 acne,28,29 gout,30,31 erectile dysfunction,32 polycystic ovarian syndrome (PCOS)33 and depression.34 This physiological cascade, which begins with excessive carbohydrates and sugars, explains why the continuous consumption of high-glycemic foods in the Bronx creates a self-reinforcing cycle of metabolic dysfunction that standard dietary recommendations fail to interrupt.
THERAPEUTIC FAILURES: Why Conventional Approaches Fall Short
The standard advice of “eat less, move more” has been followed consistently since becoming official government guidance in 1977.35,36 Given that insulin resistance is the underlying cause of diabetes and the primary contributing macronutrient is carbohydrates, it is no surprise that current guidelines—which suggest minimizing fat and deriving roughly 45-65% of calories from carbohydrates—have failed to help people.36
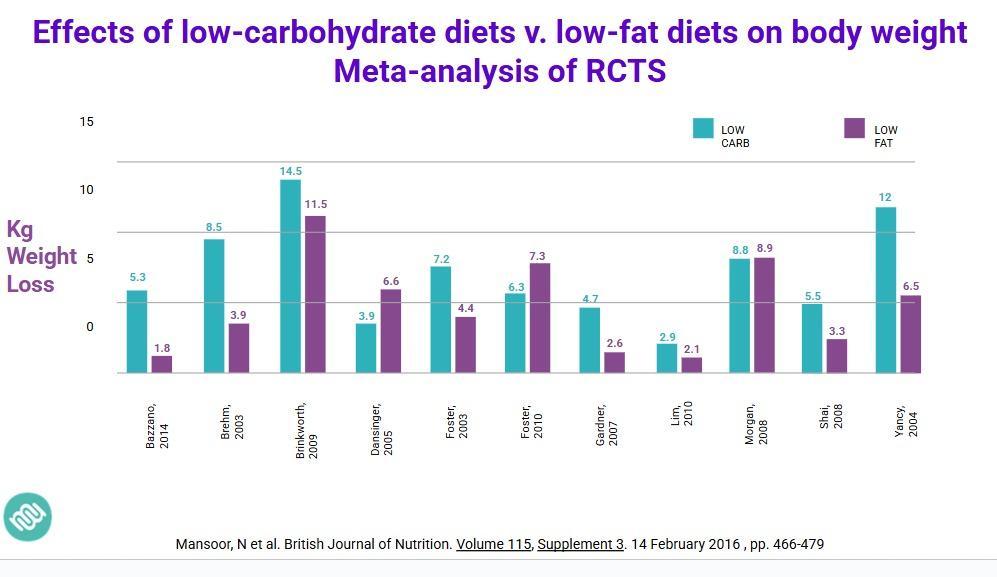
Figure 2: Meta-analysis across clinical trials comparing diets to body weight37
Research shows that individuals following calorie-restricted, high-carbohydrate diets experience higher hunger scores than those on carbohydrate-restricted plans with equivalent calories.38 The LookAHEAD trial, which used calorie restriction with intensive lifestyle intervention, failed to show significant cardiovascular benefits despite modest weight loss.39 Calorie restriction without addressing macronutrient composition leads to decreased energy expenditure and increased hunger,40 making this approach unsustainable.
While valuable for overall health, exercise alone has proven insufficient to overcome the metabolic effects of high-carbohydrate diets. A meta-analysis of 9 clinical trials demonstrated that exercise without dietary modification produces only a 8% decrease in HbA1c,41 which is not impactful enough for the estimated 17-37% of the Bronx diabetes population with uncontrolled (A1c > 9%) diabetes.42,43,44
NUTRITIONAL KETOSIS APPROACH: Evidence for Metabolic Transformation
To solve the Bronx’s metabolic disorder epidemic, we must embrace innovative, evidence-based interventions that address the root dietary causes to reverse metabolic conditions. In practical terms, nutritional ketosis means a very-low-carbohydrate diet. Dozens of randomized controlled trials have shown that nutritional ketosis—achieved through significant carbohydrate reduction—represents a powerful intervention for metabolic disorders that reverses chronic disease. 45,46,47,48,49,50,51,52 This therapeutic low-carbohydrate diet shifts the body’s metabolism from burning glucose to burning fat and producing ketone bodies in the process. This approach directly targets insulin resistance by drastically reducing the intake of sugars and starches that drive blood sugar spikes.53 Unlike most diabetes programs which focus on incremental blood sugar improvements and managing diabetes over the long term, the ketogenic approach treats the root cause of the problem normalizing all of the components of the metabolic syndrome (See Figure 2 and 3). By virtually eliminating high-glycemic foods, this diet allows blood glucose levels to stabilize and insulin levels to fall, addressing the core defect in type 2 diabetes. As insulin sensitivity improves, many patients can reduce or discontinue medications (particularly insulin and sulfonylureas) under medical supervision.54 Importantly, ketosis, which is achieved when your body is only processing fats for energy, alleviates hunger and cravings and increases energy levels.55 The ketogenic/low carbohydrate diet is a disease modifying intervention.
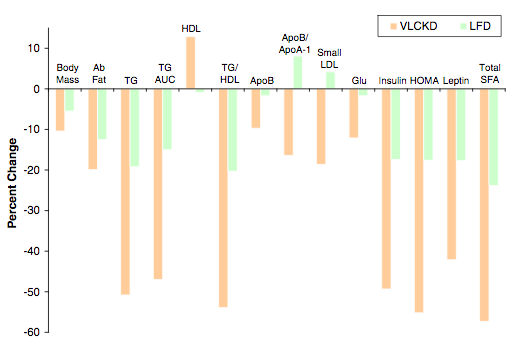
Figure 3: Low carbohydrate diets (VLCKD) perform better than low fat diets (LFD) in every metabolic parameter 56
The Virta Health trial is an open-labeled non-randomized controlled study, which showed that participants in a ketogenic program reduced their HbA1c by over 1% (absolute), with over half of the intervention group achieving diabetes remission within one year while reducing medications by 67%.57 In his UK practice, Dr. David Unwin has shown that a low-carbohydrate diet delivered in primary care can lead to type 2 diabetes remission in nearly 50% of patients, with an average weight loss of 8.3 kg, and significant reductions in diabetes medications.58 Dr. Glandt’s clinical practice has also documented significant improvements in glucose control in populations with long term standing diabetes [average of 12 years] (See Figure 4), while decreasing medications, particularly a 79.5% decrease in insulin use.59 This experience is also being replicated by OwnaHealth in the Bronx patient population, with 2.1% absolute reduction in A1c.60,61 (See testimonials from the Bronx)
These real-world results highlight that lifestyle change can be a powerful tool for managing and reversing type 2 diabetes.
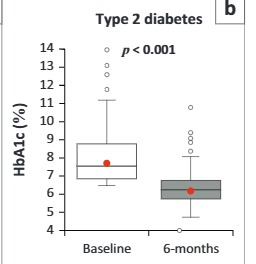
Figure 4: Baseline and 6-month follow-up haemoglobin A1c (HbA1c) in patients with type 2 diabetes (HbA1c > 6.5%)59
Fortunately the American Diabetes Association has acknowledged since 2019 that low-carb and very-low-carb eating patterns “have demonstrated the most evidence for improving glycemia” and are legitimate options for patients.62 Moreover, the Peterson Health Technology Institute, an independent nonprofit organization, reported that of all digital diabetes management solutions evaluated, nutritional ketosis-based programs demonstrate better glycemic control and higher potential for diabetes remission compared to all other existing digital diabetes management solutions.63
CALL TO ACTION: Transforming Metabolic Health in the Bronx and Beyond
The evidence clearly demonstrates that the Bronx’s metabolic health crisis—reflective of America’s broader metabolic dysfunction—requires a paradigm shift in our approach. Implementation requires comprehensive community education, food access solutions, cooking skills development, and healthcare integration, all tailored to the specific socioeconomic and cultural context of the Bronx.
Crucially, any solution must be scalable and sustainable. Nutritional ketosis has the advantage that, once education and initial support are provided, the ongoing “maintenance” (i.e., eating real food) is cost-effective. Patients often save money by cooking at home and avoiding expensive processed snacks.64 As their health improves, healthcare expenditures on medications and emergency care go down—potentially freeing resources to reinvest in prevention. As of 2022, which pre-dates the sharp rise in use of GLP-1 agonists, 10% of total healthcare budgets were spent on diabetes and its complications.65 If remission-driven diets were implemented largely, the healthcare savings would be enormous.66,67
We call upon policymakers, healthcare leaders, and community stakeholders to support the Bronx Project’s implementation of evidence-based nutritional interventions that can transform one of America’s most metabolically challenged communities into a model for nationwide intervention.
Dr. Mariela Glandt, a Harvard and Columbia-trained endocrinologist with over 20 years of experience, transforms diabetes care as co-founder of OwnaHealth and the Glandt Center, leveraging ketogenic diets, innovative technology, and low-carb solutions to reverse type 2 diabetes and promote metabolic health globally.
Article Reference: South Bronx – References





