
Veterans
The Metabolic Health Epidemic in U.S. Veterans: Prevalence, Etiology, Impact, and Interventions
Seventy-five years ago, the VA was forged to safeguard our service members’ health in a world where chronic disease was a rarity; today, a staggering 90% of its budget is consumed battling the relentless tide of chronic conditions afflicting our veterans.
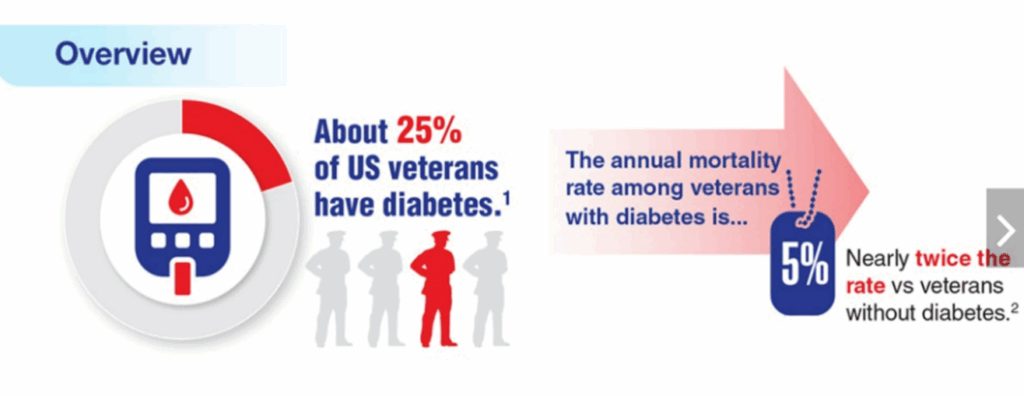
Metabolic health in the United States is a growing concern, particularly among military veterans. Veterans, a group already at higher risk due to their unique experiences and health challenges, face a disproportionate burden of metabolic disorders such as obesity, type 2 diabetes, and related cardiometabolic disorders [1] [2] [3]. The costs are staggering at $1.5 billion a year on diabetes care [4]. Only 6.9% of VA patients are metabolically healthy lean (MHL) [5]. The poor state of metabolic health among veterans is the result of various factors, including the physical and psychological toll of military service, limited access to healthcare, and lifestyle challenges that persist after their service. Addressing these issues requires a multifaceted approach that involves improving care access, promoting healthier lifestyles, and integrating mental health support into physical health programs [6] .
Source: https://www.healthquality.va.gov/guidelines/cd/diabetes/
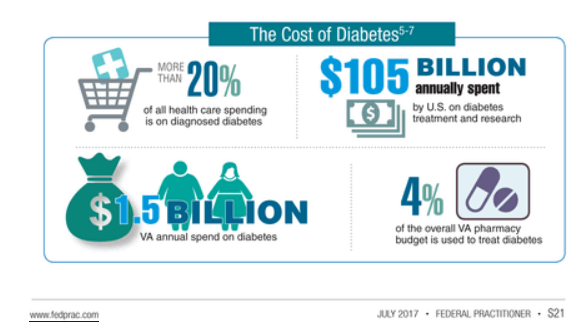
Source: https://www.fedprac-digital.com/federalpractitioner/data_trends_2017
Prevalence of Metabolic Dysfunction
Over 40% of veterans are obese, with rates exceeding 50% among those aged 45–64 [7]. These conditions are not only linked to a range of chronic diseases, including heart disease and stroke, but they also significantly reduce quality of life and life expectancy [8] [9].
Diabetes prevalence among veterans rose from 15.5% in 2005–2006 to 20.5% in 2013–2014 [10]. In high-risk regions like Martinsburg, West Virginia, 31% of veterans have diabetes (Diabetes Week 2024 data).
Unfortunately, veterans are at a significantly higher risk for poor metabolic health, with numerous studies showing that they are more likely to experience these conditions than their civilian counterparts [11]. This trend has serious implications for the overall health and well-being of veterans, especially as they age.
Contributing Factors to Poor Metabolic Health in Veterans
a. Physical and Mental Health Strain from Military Service
Military service is physically demanding and often involves long deployments, strenuous physical activity, and exposure to harsh environments. While many service members are in peak physical condition during their active duty, the physical toll of service can contribute to long-term health problems. For example, veterans often suffer from musculoskeletal injuries, which can make it harder to maintain physical activity levels once they leave the military [12] [13]. This can lead to a sedentary lifestyle, weight gain, and the onset of metabolic diseases.
Moreover, military personnel are at higher risk for mental health issues such as post-traumatic stress disorder (PTSD) [14], depression [15] [16], and anxiety [17]. These conditions are known to have a significant impact on physical health, often contributing to poor metabolic outcomes [18] [19] [20]. PTSD, for example, has been linked to higher rates of obesity and diabetes due to its effect on stress hormones, sleep disturbances [21] [22], and emotional eating [23]. The psychological toll of military service can make it more difficult for veterans to adopt healthy behaviors, further exacerbating their risk for metabolic disorders [24].
A study in JAMA Psychiatry used GrimAge, a biomarker of biological age, to assess the impact of PTSD and obesity on aging in veterans. It found that veterans with PTSD were twice as likely to experience accelerated aging. The combination of PTSD and obesity significantly increased this risk, likely due to stress, inflammation, and metabolic factors. [25] [26] [27] [28] [29]
Blast Exposure (BE) disrupts hypothalamic-pituitary-adrenal (HPA) axis function, increasing cortisol production and insulin resistance [30] [31]. Veterans with BE exhibit 2x higher risk of glucose dysregulation, independent of PTSD or TBI. Traumatic Brain Injury (TBI) alters appetite-regulating hormones (leptin, ghrelin) and promotes visceral fat accumulation [32]. Alcohol and opioid misuse worsen dietary habits, liver function, and insulin sensitivity.
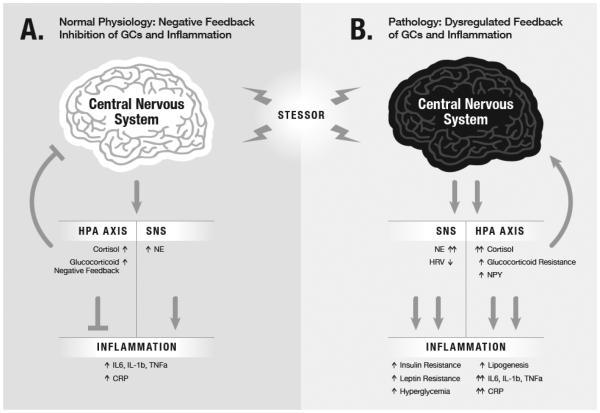
Image: Posttraumatic stress disorder: A metabolic disorder in disguise? (ref 19)
b. Lifestyle Changes After Service
When veterans transition from military to civilian life, they often face challenges that impact their ability to maintain a healthy lifestyle. The structure and discipline that come with military service can be difficult to replicate in civilian life, and veterans may struggle to establish routines that promote good physical health[33]. Additionally, veterans may experience challenges related to social support, which can be a critical factor in maintaining health and well-being. Without the camaraderie and support of military peers, veterans may feel isolated, leading to unhealthy coping mechanisms such as overeating, alcohol use, or smoking.
Veterans may also face financial instability, which can make it harder to afford healthy food and access to healthcare. These challenges are particularly prevalent among veterans who are younger or who did not have high-paying roles in the military[34]. Financial difficulties can lead to poor dietary choices, which contribute to the development of metabolic conditions like obesity and diabetes. Veterans with <12 years of education have a 33.5% diabetes rate vs. 19.9% in college-educated peers [35] .
c. Barriers to Healthcare Access
Although veterans are entitled to healthcare through the Department of Veterans Affairs (VA), access to care is not always straightforward. Veterans often face long wait times for appointments [36] [37], especially in rural areas where VA facilities may be limited [38]. This can delay diagnosis and treatment of metabolic disorders, leading to worsened outcomes. Additionally, the VA system is often overwhelmed, which can result in veterans not receiving the comprehensive care they need to address their metabolic health.
Furthermore, the care provided may not be holistic. Veterans may receive treatment for one condition (e.g., high blood pressure), but their broader health needs, such as mental health or nutrition counseling, may be overlooked. This lack of comprehensive care makes it harder for veterans to manage their metabolic health effectively.
The Impact of Poor Metabolic Health on Veterans’ Lives
The consequences of poor metabolic health among veterans are far-reaching. Veterans with obesity and diabetes are at a higher risk for cardiovascular disease, kidney failure, amputations, and other debilitating conditions. They are also more likely to experience reduced mobility, chronic pain, and decreased quality of life. These physical issues are compounded by mental health challenges, creating a vicious cycle where poor physical health exacerbates mental health problems, and vice versa.
Additionally, poor metabolic health can have a negative impact on veterans’ economic stability. Veterans who are in poor health are more likely to face difficulties in maintaining employment, leading to financial strain. This, in turn, can limit their ability to afford healthy food, medications, and other resources necessary for managing their conditions.
Current Interventions and Limitations
The VA has implemented several programs to address metabolic health issues among veterans, but these initiatives face significant challenges. The CREW Program (Asheville VA) is a structured 16-week intervention that integrates low-carb nutrition (<100g carbs/day), medication deprescribing, and whole health coaching. Early results have been promising, with participants experiencing an average 15-lb weight loss and a 0.71% reduction in HbA1c, while 61% reduced or eliminated diabetes medications [39]. Dr. Mark Cucuzzella has achieved similar results using a comparable approach within the constraints of a busy primary care setting, as demonstrated in an IRB-approved research project involving over 450 veterans with a 12-month follow-up. Dr Dina Griauzde 12 month pilot with carbohydrate reduction shows promise. The mean percent weight loss was 9.4% with 9 participants (50%) achieving ≥5% weight loss [40]. Using a similar dietary approach, Virta Health has also completed a successful pilot study with the aim of obesity and diabetes reversal [41].
The Mission of Dr. Mark Cucuzzella’s Clinic at the Martinsburg VA
However, broader VA initiatives like the MOVE! Weight Management Program, which emphasizes calorie restriction and physical activity, have shown limited long-term success. Despite the widespread availability of MOVE!, rates of participation remain low [42] [43] and most participants (≥ 75%) do not achieve ≥5% weight loss within 12 months [44] [45] [46]. Additionally, gaps in care persist, including outdated nutritional guidelines that favor low-fat diets over evidence-based low-carb approaches. Another major limitation is provider education—few VA clinicians receive nutrition-focused training, leaving many veterans without access to informed dietary guidance. Addressing these gaps is critical for improving long-term metabolic health outcomes for veterans.
Improving metabolic health is hindered by misaligned metrics and incentives that focus on treating numerical markers—such as hemoglobin A1C, blood pressure, and lipid levels—rather than addressing the root causes of disease. This approach is akin to turning off a flashing red light that warns of a hole in the road; it doesn’t fix the underlying problem but instead creates a false sense of security. There is a fundamental difference between pharmacologically altering a biomarker and making physiological changes that address the disease itself. Chronic disease management is complex and requires a more nuanced approach beyond simply adjusting numbers.
Forging the Path Forward: Advancing Metabolic Health for U.S. Veterans
To improve the metabolic health of veterans, a comprehensive approach is required. VA Whole Health [47] has tried to address this but it’s not widely implemented. The VA system must improve access to care, especially in underserved areas. The VA must integrate mental health services, nutritional and lifestyle counseling, and the medical team in a coherent plan to improve metabolic health.

Image: VA Whole Heath https://www.va.gov/wholehealth/circle-of-health/index.asp
Additionally, there needs to be greater emphasis on prevention [48]. Public health campaigns targeted at veterans could promote healthier lifestyle choices, such as regular physical activity, lower carbohydrate diets for metabolically compromised veterans, and stress management techniques. Encouraging veterans to engage in regular exercise and to seek help for mental health issues could go a long way in reducing the prevalence of metabolic diseases. Addressing the financial barriers to healthy living is crucial. The VA could explore options for subsidizing healthy food options. This would help alleviate some of the economic burdens that prevent veterans from managing their metabolic health effectively.
Call to Action
The poor state of metabolic health among veterans is a pressing issue that demands immediate attention. Veterans face unique challenges that put them at higher risk for metabolic disorders, including physical and mental health struggles, lifestyle changes after service, and barriers to metabolic health care. Addressing these challenges requires a holistic approach focusing on metabolic and mental health. Only through such a multifaceted approach can the metabolic health of veterans be improved, leading to better outcomes for this deserving population.
Dr. Mark Cucuzzella, a retired Air Force Lieutenant Colonel and primary care physician at the Martinsburg VA is revolutionizing metabolic medicine and diabetes care for veterans through low-carbohydrate interventions, continuous glucose monitoring, and evidence-based protocols that have demonstrated significant improvements in weight, HbA1c levels, and medication reduction for patients with type 2 diabetes.
Dr. Mark Cucuzzella, a retired Air Force Lieutenant Colonel and primary care physician at the Martinsburg VA is revolutionizing metabolic medicine and diabetes care for veterans through low-carbohydrate interventions, continuous glucose monitoring, and evidence-based protocols that have demonstrated significant improvements in weight, HbA1c levels, and medication reduction for patients with type 2 diabetes.
…………………
*Appendix: Video presentation on the topic by the author
Combat Veterans and Metabolic Illness- Can a Brief Intervention Create Retreat






