
Polycystic Ovarian Syndrome and Infertility
A National Crisis in Women’s Health: PCOS and Metabolic Infertility
Infertility is a major health crisis in the United States, rising each year without remission. Over the past 20 years, infertility has exploded from 1 in 10 couples unable to achieve pregnancy to currently 1 in 6. Fueling this increase is the number one cause of infertility in the United States: Polycystic Ovarian Syndrome (PCOS). PCOS is not only a gynecologic condition – it has become the number one hormonal disorder of women in the US affecting over 15% of all reproductive aged women. It devastates the health of women in every organ system and at every stage of their life, before, during, and beyond their reproductive years. Currently PCOS is diagnosed by reproductive criteria, yet the root causes lie in systemic metabolic dysfunction.
Root Cause of Infertility in Women: Metabolic Dysfunction
Polycystic ovarian syndrome is now recognized as an endocrine metabolic disorder and its rise in incidence is fueled by the same environmental, lifestyle, and dietary factors that have led to increases in obesity, cancer, and heart disease. For women with PCOS, it brings a lifelong burden of disease, including dramatically increased risks for type 2 diabetes, cancer, cardiovascular disease, pregnancy complications, and mental health disorders.
Behind its epidemic rise in rates are the modern US dietary, environmental and behavioral factors. Diets high in refined carbohydrates and ultra-processed foods, sedentary lifestyles, and a medical system that too often addresses symptoms rather than root causes. Its genetic and hormonal roots have remained unchanged – at the core of its rising rates is the insulin resistance, frequent obesity, and chronic inflammation that drives the risk factors to become clinical disease.
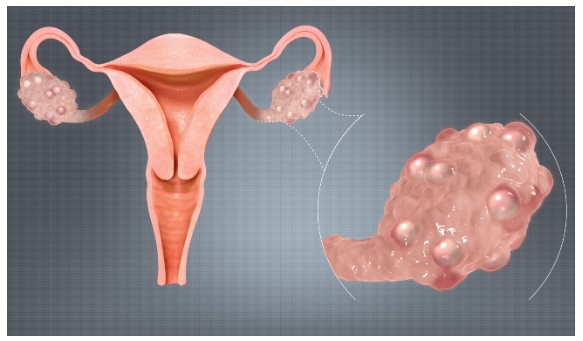
The core diagnosis of PCOS requires two of three factors: (1) absent ovulation; (2) more than 20 ovarian cysts; and (3) elevated male hormones. Common symptoms include severe acne and male pattern hair growth on the face, chest, lower abdomen, thighs, or male pattern baldness, obesity, irregular menstrual cycles, and depression and mood disorders.
At the heart of PCOS is insulin resistance.
In over 70% of women with PCOS— including those with it who are lean—cells become resistant to insulin’s effects and the pancreas compensates by secreting more insulin. This excess insulin drives the ovary to make androgen hormones that further disturb ovulation, suppresses hepatic male hormone binding protein SHBG, further raising androgen levels in the blood, and driving more insulin resistance. The result is not just irregular menses and infertility but a vicious feedback loop where worsening metabolism exacerbates hormonal dysfunction, and vice versa.
- 70–80% of PCOS patients exhibit insulin resistance, including 30–50% of lean women with PCOS.
- One half of women with PCOS will develop diabetes by age 40.
- Women with PCOS have nearly 3x the risk of gestational diabetes.
- PCOS women have a 4–5x increased risk of type 2 diabetes.
- Up to 85% of anovulatory infertility is due to PCOS.
- Up to 55% of women with PCOS have metabolic associated “fatty liver” (MASLD) now the #1 cause of liver transplant in the USA.
- PCOS-related healthcare costs in the U.S. are estimated to exceed $4 billion annually, excluding long-term metabolic complications.
The Metabolic-Hormonal Cascade: A Vicious Cycle
- Elevated insulin → ↑ Androgens (male hormones via ovarian stimulation)
- ↑ Androgens → Blocked ovulation, hirsutism, acne
- Visceral Fat Gain → ↑ Inflammatory cytokines → More insulin resistance
- Reduced SHBG (androgen binding proteins)→ worsened hormonal imbalance

Misguided Treatments and Policy Failures
Conventional Errors:
- Emphasis on pharmacologic management of symptoms (birth control pills, IVF) without addressing metabolic roots.
- Calorie-counting without macronutrient restructuring has led to poor long term outcomes.
- Failure to adequately diagnose a majority of those affected.
- Nutritional guidelines for PCOS remain vague and outdated, often promoting high-carb, low-fat diets despite strong evidence that these worsen insulin resistance.
The symptoms of PCOS are conventionally treated with birth control pills. Oral contraceptives suppress male hormone levels, but do not treat the underlying cause and are a lifelong therapy that once stopped lose efficacy.
Conventional fertility treatments are expensive, often drastic interventions for a disease that can be effectively reversed through lifestyle and diet. Oral drugs that help to trigger ovulation work in less than half of patients and can cause high-risk multiple pregnancies. Insulin sensitizing diabetes drugs such as metformin have increasingly been added with limited results.
In vitro fertilization (IVF) is a successful but expensive and invasive treatment for infertility, including metabolic infertility and PCOS. A woman is given injectable fertility medications to trigger the development of 10 to 20 eggs, which are surgically extracted from the ovary and fertilized with sperm to create multiple embryos that are grown outside of the body. This is highly effective treatment, but can cost upwards of $25,000 per month, requires daily injections and surgical procedures, and leads to the creation of excess fertilized embryos in long term storage.
IVF treats infertility, but it does not address metabolic dysfunction. When the woman is metabolically unhealthy, even successful fertility treatments can lead to high-risk pregnancy and catastrophic outcomes for the mother and her baby.
Success rates are lower for metabolically unhealthy fertility patients, and miscarriage rates are increased. Perhaps most alarmingly, a mother’s abnormal hormonal profiles in pregnancy also affect her developing child hormonally and developmentally, leading to increased rates of diabetes and similar reproductive hormonal problems in her offspring. PCOS does not just affect the mother, but also the child.
What Works: Evidence-Based Lifestyle Interventions
Successful lifestyle management interventions have focused on dietary carbohydrate restriction. Clinical programs focusing on coaching and education can ameliorate and often reverse PCOS associated infertility in a matter of months.
Overcome PCOS™ is an online program that provides lifestyle and nutritional coaching and education to reverse the metabolic and hormonal abnormalities of PCOS. Through social media and by incorporating Overcome PCOS™ into clinical treatment protocols, Dr. Palter at Gold Coast IVF in Woodbury, NY has improved clinical outcomes for traditional infertility patients and has reported spontaneous pregnancy for women following the Overcome PCOS™ protocol. Clinical outcomes have shown rapid reduction in insulin resistance, inflammatory markers, weight and higher rates of spontaneous ovulation and pregnancy.
A pilot study of a dietary program by Cincione, 24 overweight women with PCOS were randomized to follow either a very-low-calorie ketogenic diet or a hypocaloric
Mediterranean-style diet for 12–16 weeks. The ketogenic diet group achieved a 13.7% reduction in BMI, compared to just 5.1% in the Mediterranean group (p = 0.0003). More
importantly, the ketogenic group saw significantly larger reductions in waist circumference, fat mass, and serum free testosterone (−30.4% vs −12.6%). The ovulation rate more than doubled in the ketogenic group, jumping from 38.5% to 84.6% by week 16. Insulin resistance, measured by HOMA-IR, also improved by 23%.
These findings were echoed in a 2023 study by Pandurevic where a ketogenic protocol was tested against a standard low-calorie diet in 27 obese women with PCOS. The ketogenic group again showed superior results: body fat dropped by 24%, SHBG increased significantly, and free testosterone fell by 30%—more than double the reduction in the control group. Ovulation improved in 85% of the ketogenic group, compared to just 36% of the conventional diet arm.
In study RCT by Mei et al., a Mediterranean/low-carb hybrid diet produced greater reductions in body fat and fasting insulin than a low-fat diet. Total testosterone dropped only in the lower-carb group, and menstrual regularity was restored in 87% of women on the MED/LC diet.
A Meta-analysis of dietary interventions (Khalid et al., 2023): Pooled data from 7 trials showed consistent improvements in weight, LH/FSH ratio, free testosterone, and SHBG.
A hypocaloric high-protein, moderate-carb diet Nadjarzadeh et al. (2021): did not outperform standard diets when calories were matched—highlighting the importance of carbohydrate quality and patient phenotype (especially insulin resistance).
These findings suggest that insulin control—achieved via diet—is a critical therapeutic target in PCOS.
Call to Action: A Metabolically Sensitive Public Health Strategy
To end the chronic disease crisis, we must:
- Redefine PCOS as a metabolic disease.
- Incorporate dietary carbohydrate reduction into national guidelines for insulin resistance and PCOS.
- Invest in long-term clinical trials comparing dietary patterns with pharmacologic interventions.
- Update public nutrition recommendations to reflect modern evidence on the harm of excess refined carbohydrates.
- Integrate PCOS into broader metabolic disease policy initiatives (e.g., T2DM, obesity prevention in youth).
PCOS affects millions of American girls and women, often during their peak reproductive and working years. It is both underdiagnosed and poorly treated—too often managed with oral contraceptives and anti-androgens that suppress symptoms rather than targeting underlying metabolic dysfunction. Many of these patients go on to develop diabetes, cardiovascular disease, cancer, or chronic infertility—burdens that are largely preventable.
To reverse the chronic disease epidemic, we must start where the problem begins: in the metabolic derangements of youth. Dietary and lifestyle interventions—when properly applied—can restore American girls and women to reproductive and metabolic health.
Dr. Steven Palter, founder and medical director of Gold Coast IVF, is changing the paradigm of PCOS treatment by emphasizing lifestyle and dietary interventions to target insulin resistance, recognizing PCOS as a hormonal and metabolic disorder that has become the leading cause of infertility.
Article Reference: PCOS and Infertility – References





