
USDA Dietary Guidelines for Americans
Why Does America Have Chronic Disease Epidemics?
and
Why Reform of the US Dietary Guidelines is the Key Policy to Reverse These Diseases
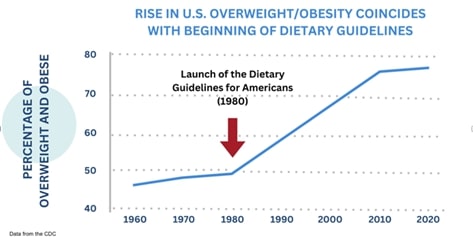
In 1960, Chronic Disease Was Rare in America. We did not always suffer from chronic diseases. In 1900, America had few cases of heart disease, obesity, diabetes, or cancer. In 1960, the adult obesity rate was 9.6%[1]. That rose to 42.4% in 2018 (latest government data) [2]. Today, the obesity rate is likely close to 50%. Beyond obesity, rates of all diet-related chronic diseases have skyrocketed. In 2014, 60% of American adults had one or more of these diseases (60% is the CDC’s latest number; it has not been updated [3],[4]). An outside estimate put that rate at 88% in 2018 [5]. Today, we cannot even remember being disease-free. Sickness is ubiquitous.
Three Major Events Explain Our Disease Epidemics:
First, in 1961, the American Heart Association (AHA) issued the first-ever policy anywhere in the world advising the public to avoid saturated fat and dietary cholesterol as the best strategy for preventing heart disease [6]. Food-wise, this meant eating fewer/less eggs, butter, cheese, red meat, and whole milk. These would be replaced by chicken, low-fat cheese, margarine/seed oils, and, to a large extent, grains. This policy was based on a single, unpublished—yet enormously influential–study (the renowned “Seven Countries Study” [7]) by the researcher Ancel Keys. Keys had developed the “diet-heart hypothesis,” [8] i.e., that saturated fat and cholesterol cause heart disease, and in the Seven Countries Study, he set with a strong bias to prove that he was right [9].
To achieve this goal, Keys cherry-picked the countries he studied, selecting Italy, Greece, and Yugoslavia where people ate little meat and dairy (due to disruptions from WWII) and had low rates of heart disease [10]. Meanwhile, Keys avoided countries like Switzerland and France, where people also had low rates of heart disease yet ate far more meat and dairy. Keys knew that including these countries would disprove his hypothesis, so he left them out. Keys also visited Greece during Lent, where a strict Orthodox fast meant that no animal foods were eaten [11]. The Lent data skewed the study results, making it seem as if the Greeks barely ate animal foods—far from the truth. Yet, no one realized these and other flaws in the study at the time. The unprecedented size and scope of Keys’ study—on nearly 13,000 men–made him famous and landed him on the cover of Time magazine. Always aggressive and self-promoting[12], Keys persuaded the AHA to adopt his idea. The AHA thus told the entire nation to cut back on saturated fat and cholesterol based on Keys’ flawed data. Today, we are still living with the misguiding idea of this crusading scientist.

The second event to promote our disease epidemics was the “low-fat” diet. This diet cuts back not just on saturated fat but all fat. The AHA also introduced a “low-fat” policy in 1970, stating that fat contains nine calories/gram, whereas protein and carbohydrates only contain 4-5 calories/gram [13][14]. However, the low-fat diet had virtually never been tested in a clinical trial. A diet low in fat, saturated fat, and cholesterol has been a vast uncontrolled experiment on the American population, without our consent.
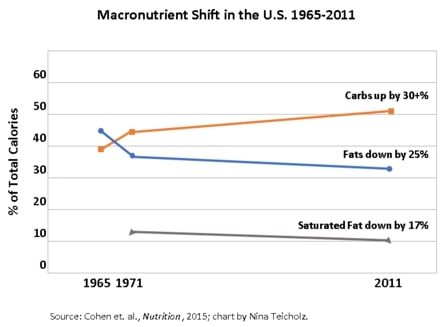
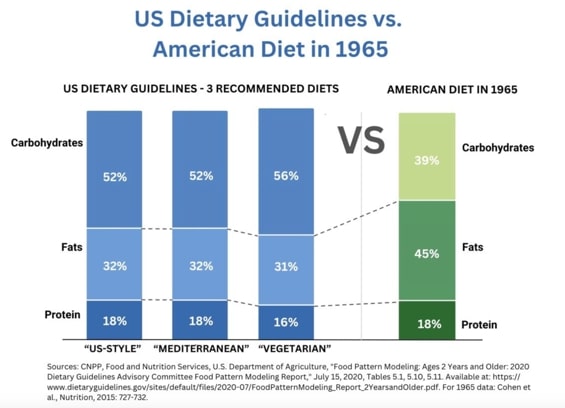
Removing fat from foods inevitably means increasing carbohydrates, because cutting meat, dairy, and eggs leaves few options—mainly pasta and cereals. The low-fat diet also led to the “Snackwell’s effect,” i.e., cookies loaded with sugar and marketed as healthy due to their low-fat content. From 1965-2011, Americans reduced their fat consumption by 25% as a percent of total calories while increasing carbohydrates by 30% [15]. (Note that carbohydrates drive seesawing blood-sugar levels and therefore provoke cravings, causing people to overeat; by contrast, protein and fat are far more satiating [16].)
The third event to cause our epidemics occurred in 1980, when the USDA-HHS launched the US Dietary Guidelines for Americans. This policy adopted the entire dietary platform of the AHA. The guidelines quickly became the North Star for eating in America, with unsurpassed influence. These guidelines drive the National School Lunch Program, feeding programs for the elderly, hospital meals, and even food for the military (which has an obesity rate equal to the general population) [17]. The guidelines are also downloaded by most health professionals as the virtual gold standard. The result has been a sharp upward turn in obesity rates.
Do the Dietary Guidelines Protect Against Chronic Disease?
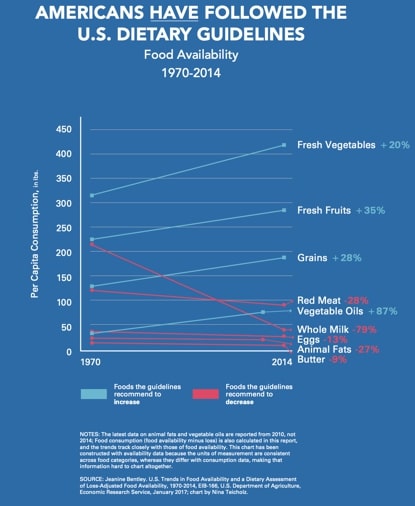
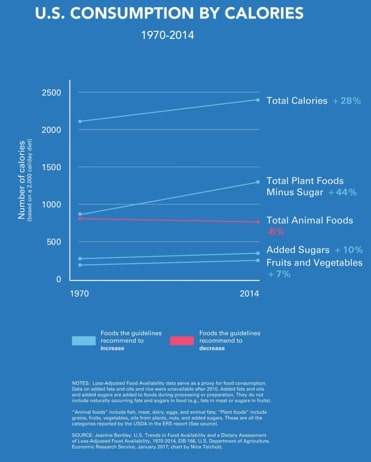
A common defense of the Dietary Guidelines is that they do promote good health but that the public fails to follow them. This argument is contradicted by the best-available government data, which show that Americans have complied with nutrition guidelines perfectly, in every food category measured [18]. Most notably, Americans have increased consumption of fruits, vegetables, and grains (mostly whole grains; refined grains have declined since 1999 [19]), while red meat, whole milk, eggs, and butter are eaten far less. Beef consumption has declined by 35% from 1970 to 2014. This historical evidence shows that further increases in plant foods to replace animal foods are not a proven formula for preventing chronic disease.
Rigorous Tests of the Dietary Guidelines Found No Health Benefit. The Dietary Guidelines Process Has Ignored All These Results
The National Institutes of Health (NIH) has spent billions of dollars on large, randomized, controlled clinical trials (the most rigorous type of evidence) to test the effectiveness of a diet low in saturated fat, total fat, and cholesterol. These trials include the largest clinical trial ever conducted in the history of nutrition science on 49,000 women, called the Women’s Health Initiative (cost: $725M). Half of these women were told to follow the guidelines, which they did—successfully decreasing their fat intake from 37 to 29% of calories [20]. They also reduced their saturated fat, cholesterol, and meat intake compared to controls. However, after seven years, the women on a diet saw no benefit in preventing heart disease [21], type 2 diabetes [22], or cancer of any kind [23]. They also weighed only 2 pounds less than the controls [24]. Worse, a follow-up study found that postmenopausal women on the low-fat diet suffered from higher rates of heart disease [25].
In 2000, the Dietary Guidelines Advisory Committee (DGAC) expressed concern that the government’s low-fat advice “could engender an overconsumption of total calories in the form of carbohydrates, resulting in the adverse metabolic consequences of high-carbohydrate diets” [26]. The expert report added, “Further, the possibility that overconsumption of carbohydrates may contribute to obesity cannot be ignored.”
In 2015, the DGAC report explained that dietary advice should not emphasize reducing total fat [27], because low-fat “diets are generally associated with dyslipidemia (hypertriglyceridemia and low HDL-C concentrations)” [28], which indicates increased risk for heart disease.
Alarmingly, the Dietary Guidelines cannot even outperform the “typical American diet” (TAD). In a well-controlled clinical trial, subjects (women) were assigned to either the Dietary Guidelines or the TAD diet [29]. The TAD women received more saturated fats, 3 ½ more servings of grains per day, and more sugar, including lemon cheesecake and “Jelly Bellies” as an “all-day condiment.” The other group of women followed the Dietary Guidelines almost perfectly. Yet, at the end of the eight-week trial, those following the guidelines saw no improvements in markers of diabetes, heart disease, or blood pressure compared to the TAD group [30].
These and other clinical trial results, including all the major trials on saturated fats, have either been ignored or improperly discounted in the Dietary Guidelines reviews of the science [31].
Do the Dietary Guidelines Cause Chronic Disease?
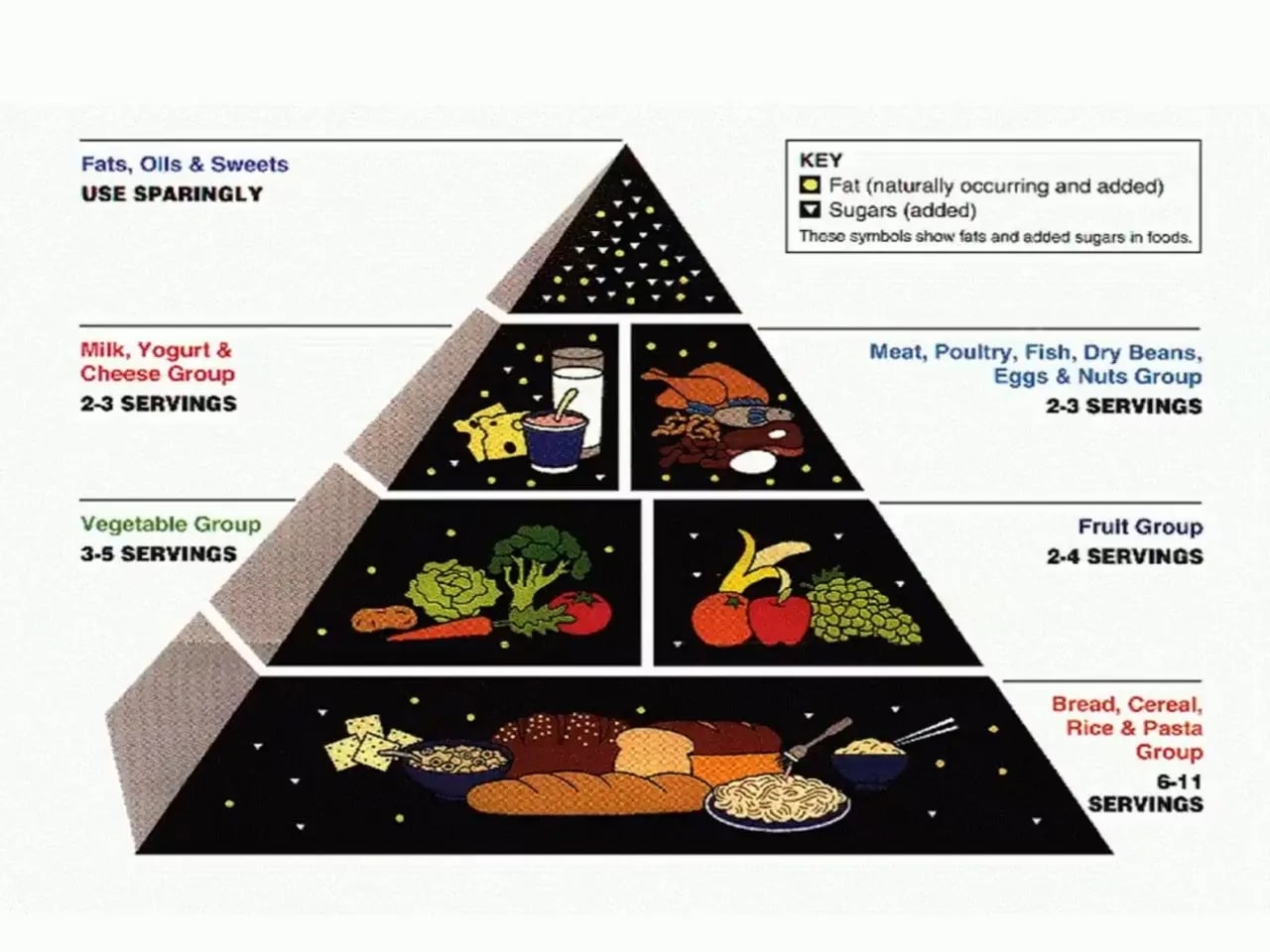
The original food pyramid shows grains and other starches in its big bottom slab. These guidelines are “high-carbohydrate,” compared to what Americans ate in 1965 [32][33], before the epidemics of chronic disease. Carbohydrates are made up of mostly glucose and fructose, each of which has an effect: (1) glucose causes the pancreas to release insulin, the king of hormones for making people fat [34].
Over time, with excessive carbohydrate consumption, the body’s ability to deal with insulin is exhausted, leading to insulin resistance, which is now widely thought to be the root cause of all chronic diseases in adults [35][36] and children [37]; (2) fructose is handled by the liver and also contributes to obesity, diabetes, and non-alcoholic fatty liver disease (NAFLD/MAFLD) [38]. More than 200 clinical trials now demonstrate that reducing carbohydrates can reverse type 2 diabetes, obesity, heart disease [39], NAFLD/MAFLD, and other chronic diseases, often within just weeks. Additionally, low-carbohydrate diets have been shown to be safe (without side effects), sustainable, and affordable [40]. The Dietary Guidelines process has ignored and suppressed the entire scientific literature on low-carbohydrate diets [41].
Other Unhealthy Requirements in the Guidelines
- The guidelines require that seed oils supply all added fat despite the well-documented effects of these fats on oxidation [42], inflammation, and heart disease [43].
- The cap on saturated fats (10% of calories) limits protein-rich, nutrient-dense foods, including cheese, meat, and eggs.
- The excessively low limit on sodium (230 milligrams) is at a level that has been documented to increase the risk of heart disease [44],[45],[46],[48].
- The protein requirement (0.8 grams per kg of body weight) meets only minimal requirements for survival. It is far below the level (1.2–1.6 grams) required for weight loss, muscle maintenance, serious illness recovery [48], and overall well-being [49], especially for children [50] and older adults [51].
Dietary Guidelines Do Not Meet Basic Nutritional Needs
Even if followed perfectly, the Dietary Guidelines do not provide the essential nutrients for proper growth development and optimal health. The 2020 Dietary Guidelines Expert Report states: “Nutrients that do not meet Recommended Dietary Allowance or Adequate Intake goals include the following: Iron, Vitamin D, Vitamin E, Choline, and Folate” [52].
Is There Particular Harm to Children?
- There is currently no limit to the amount of sugar served to children in the National School Lunch Program.
- School lunches require only 2 “ounce equivalents” of protein per child, below the level necessary for normal growth and development and to prevent stunting [53].
- The sodium cap in school lunches is based chiefly on data on middle-aged, hypertensive men. The guidelines’ scientific reviews presented no data on children [54].
- Only non-fat and 1% fat milk are allowed in schools; whole milk is banned due to the cap on saturated fats. However, the guidelines’ scientific reviews presented no clinical trial data on normal, school-aged children to support the idea that these fats harm children [55].
- The Dietary Guidelines Ignore the Different Protein and Nutritional Needs of Growing Children.
The Guidelines Have No Option For the 60-88% of Americans with a Chronic Disease
The mission of the Dietary Guidelines is only to prevent—not to reverse or treat–chronic disease [58]. The guidelines’ scientific reviews omit consideration of the science on disease reversal. For instance, the 2020 guidelines process reviewed only a narrow subset of the scientific literature on weight loss [59]. Congressional language in the Appropriations Report of 2024 said, “Given the increase in chronic disease, the Committee directs USDA to include in the 2025-2030 Dietary Guidelines for Americans a dietary pattern for the treatment of diet-related diseases, including obesity and diabetes, based exclusively on rigorous data” [60].
The Guidelines’ Scientific Methodology Lacks Rigor and Transparency
The National Academy of Sciences, Engineering, and Medicine (NASEM) conducted the first-ever outside peer review of the Dietary Guidelines in two 2017 reports [61][62] mandated by Congress, with a $1 million allocation. The NASEM made 11 recommendations to the USDA [63] to improve the transparency and scientific rigor of the guidelines. Without these reforms, the NASEM made clear that the guidelines would not be “trustworthy” [64].
In 2019, Congress mandated a follow-up report by the NASEM to assess if the USDA had adopted its recommendations. This two-part report [65],[66] found that “[t]he proposed analytic and methodologic improvements to the Dietary Guidelines process has largely not yet been achieved” [67]. An outside analysis found that the USDA had not fully adopted even one of the NASEM’s 11 recommendations [68]. Another analysis found that the USDA did not comply with the NASEM on conflict-of-interest disclosures and increased rigor of the scientific reviews [69].
The 2020 USDA systematic reviews were found to be “subpar” and “of critically low quality” by an international team of top methodologists published in the American Journal of Clinical Nutrition [70][71]. The USDA has provided no evidence that it upgraded its review methodology between 2020 and 2025, implying that the 2025 reviews are of similarly low quality.
A paper published in a journal of the NASEM, by authors including three former members of previous Dietary Guidelines Advisory Committees, traces the history of longstanding concern about these guidelines by top experts in the field and by Congress. It states, “the Dietary Guidelines have not fully adhered to [its] guiding documents, which has resulted in diminished independence of the expert committee in charge of evaluating the science for the DGA and a continued lack of a fully rigorous scientific process for producing consistent and trustworthy guidelines for the public.”
CALL TO ACTION
Given the failure of the Dietary Guidelines to prevent chronic diseases, the documented lack of scientific rigor and transparency in the Guidelines process, and the large bodies of science ignored or discounted by the Guidelines, reform of this highly influential policy is imperative to improve health in America. Principal reforms would include the re-evaluations of: the cap on saturated fat, the cap on sodium, the inclusion of seed oils, the lack of nutritional adequacy, and the lack of adequate protein. In addition, the Guidelines urgently need a low-carbohydrate option for Americans with chronic diseases.
No further study of the Guidelines is needed. The NASEM reports and major scientific papers have established a foundation for immediate reform. Further, sufficient evidence supports a low-carbohydrate option for a nationwide recommendation [72].
Nina Teicholz, Ph.D., a Stanford and Oxford-educated science journalist, PhD in Nutrition, and bestselling author of The Big Fat Surprise, has transformed nutrition science by challenging conventional views on dietary fats and founding the Nutrition Coalition to align nutrition policy with rigorous, evidence-based research.
Article Reference: USDA Dietary Guidelines for Americans – References



