
Insulin Resistance and Obesity
The Metabolic Crisis
“Only 12% of American adults have optimal metabolic health—an alarming statistic that underscores the reality of insulin resistance. With up to 65% of daily calories coming from carbohydrates, often refined and ultra-processed, modern diets sustain chronically elevated insulin levels, driving insulin resistance and fueling an epidemic of chronic diseases, including heart disease, dementia, and fatty liver disease. The culprit is clear: decades of excessive carbohydrate consumption have fractured human physiology. Yet, reducing carbohydrate intake can trigger metabolic remission within weeks, restoring health where medications fail.”
Incidence
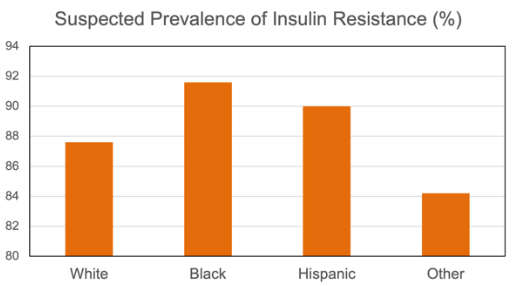
We are sick. Worldwide, people are dying from diseases that were once unheard of. Chronic diseases once considered unrelated—heart disease, Alzheimer’s, diabetes, and infertility—share a common metabolic root: insulin resistance. Nearly 90% of U.S. adults lack optimal metabolic health (Araújo et al., 2018). Black and Hispanic adults face insulin resistance rates of 90–95%, with Whites and other ethnicities closely behind. Rural areas trail urban centers by 10–15% in metabolic health, and poverty doubles the risk (CDC, 2022).
Insulin resistance is the foundation of nearly every major chronic disease. Type 2 diabetes, driven by insulin resistance in 90–95% of cases, now afflicts 34 million Americans, a 500% increase since 1980 (ADA, 2023). Alzheimer’s disease, increasingly recognized as “Type 3 diabetes,” affects 6 million and has doubled since 2000 (de la Monte, 2014). Gestational diabetes, a hallmark of severe insulin resistance in pregnancy, impacts 10% of U.S. pregnancies, doubling the rate seen in 1990, and predisposing both mother and child to lifelong metabolic struggles (ACOG, 2020; Deputy et al., 2018). Indeed, children are increasingly affected—19% of U.S. teens aged 12–19 now have insulin resistance, a condition virtually unseen in this age group in the 1970s (CDC, 2022).

In 1980, NHANES data recorded obesity, one of the most obvious indicators of insulin resistance, at 15%. Today, it stands at 42%, a steady rise that mirrors the worsening metabolic landscape (Fryar et al., 2021). Yet, despite its staggering impact, public awareness of insulin resistance remains dangerously low. A 2019 American Diabetes Association survey found that only 30% of U.S. adults recognize insulin’s broader role beyond blood sugar control, leaving the majority—especially non-diabetics—unaware of its influence on fat storage, brain health, sex hormone production, and cardiovascular function (ADA, 2019). This unawareness delays intervention, allowing insulin resistance to silently progress for years before glucose levels rise. By the time a diagnosis arrives, damage to the body is already well underway.
The evidence is undeniable: insulin resistance is the driving force behind the nation’s metabolic collapse. Addressing it is not just about preventing diabetes but reversing a crisis that impacts nearly every aspect of human health. The scale of the problem creates an opportunity: by targeting insulin resistance, it is possible to address multiple chronic diseases at once.
Disease Burden
Insulin resistance disrupts biological function at every level of life. In children, it drives visceral fat accumulation and inflammation, leading to signs of atherosclerosis by age 10 (Berenson et al., 1998; Hotamisligil, 2006). Pregnant women with insulin resistance face twice the risk of hypertension and Type 2 diabetes, while their offspring inherit a 50% higher obesity risk by adolescence (Catalano et al., 2009). In adults, insulin resistance triples cardiovascular risk, as hyperinsulinemia thickens arterial walls and accelerates plaque formation (Reaven, 2005). Non-alcoholic fatty liver disease (NAFLD) now affects 25% of Americans as insulin resistance forces the liver to both produce and retain fat (Younossi et al., 2016). In the brain, insulin resistance starves neurons of glucose, accelerating cognitive decline and increasing the risk of Alzheimer’s disease (Craft et al., 2012). Beyond these lethal conditions, insulin resistance is implicated in 70% of polycystic ovary syndrome (PCOS) cases, driving infertility and hormonal imbalances. It triples the riskeeeeta of chronic kidney disease, doubles the likelihood of depression through inflammatory cascades, and fuels erectile dysfunction by restricting blood flow and lowering testosterone (Dunaif, 1997; Chen et al., 2016; Defeudis et al., 2022).
The impact on lifespan is severe. Type 2 diabetes can reduce life expectancy by up to 10 years, while insulin resistance raises the risk of cancer, stroke, and all-cause mortality (Emerging Risk Factors Collaboration, 2011). The economic burden is immense, with diabetes alone costing $327 billion annually, straining healthcare systems and families (ADA, 2023). Insulin resistance is not a single disease—it is the unifying factor behind multiple chronic conditions. This raises the question: is insulin resistance responsible for the current generation, for the first time in recorded history, facing a shorter lifespan than their parents?
Therapeutic Gaps
Efforts to control insulin resistance fail because they target glucose rather than insulin itself. Medical guidelines focus on blood sugar markers such as HbA1c and fasting glucose, while insulin—the primary driver—remains overlooked. The same American Diabetes Association survey revealing that only 30% of adults understand insulin’s broader role explains why insulin resistance is often undiagnosed (ADA, 2019). HOMA-IR, a reliable measure of insulin resistance, is rarely tested, leaving the majority of adults undiagnosed as hyperinsulinemia persists despite normal glucose levels (Araújo et al., 2018). Furthermore, once elevated glucose reaches a level of detection, the failure to recognize the harms of elevated insulin leads to treatments that make the condition worse, such as injecting insulin itself or the use of insulin-secreting hormones.
The current rates of poor metabolic health has its foundation in dietary guidelines. Since 1977, recommendations have suggested that 45–65% of daily calories come from carbohydrates (USDA, 2020; see figure). NHANES data confirm that carbohydrate intake has averaged 51% of daily calories from 2001 to 2018, peaking near 60% in children, primarily from refined sources
such as bread, pasta, and sugary beverages (Shan et al., 2019). This constant carbohydrate consumption sustains elevated insulin levels throughout the day, driving insulin resistance (Ludwig et al., 2018). The low-fat movement of the 1980s exacerbated the issue by replacing natural fats with refined
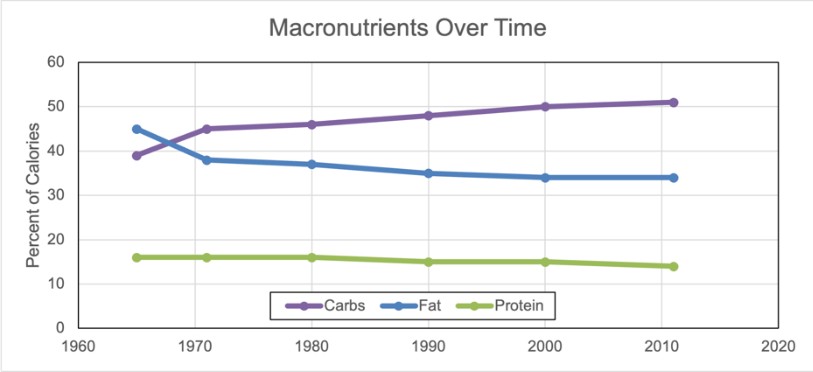
starches and sugars, further increasing insulin resistance. In gestational diabetes, treatment focuses on insulin injections rather than dietary correction, while Alzheimer’s research remains fixated on amyloid plaques, ignoring brain insulin resistance (ACOG, 2020; Craft et al., 2012). The fixation on glucose rather than insulin has resulted in ineffective treatment strategies.
Functional Remission and Prevention
Insulin resistance is not inevitable—it is highly reversible with proper interventions. Low-carbohydrate diets, defined as consuming fewer than 50 grams of carbohydrates per day, significantly reduce fasting insulin and HOMA-IR within weeks. In one study, 60% of Type 2 diabetes patients achieved remission within a year, with HbA1c dropping from 7.8% to 5.6% (Westman et al., 2008; Athinarayanan et al., 2019).
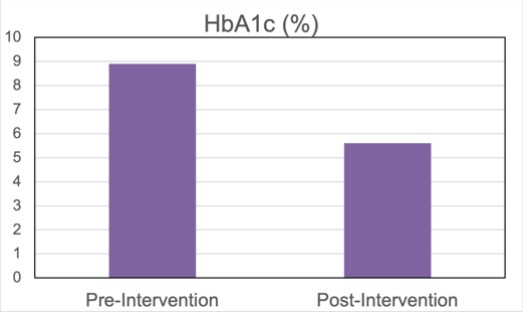
HbA1c can normalize within 90 days (Walton et al., 2019; see figure). The mechanism is clear: reducing carbohydrate intake lowers insulin demand, allowing beta cells to recover and restore insulin sensitivity (Boden et al., 2005).
In gestational diabetes, a low-carbohydrate approach halves insulin requirements, reducing preeclampsia risk by 30% and improving fetal outcomes (Mijatovic et al., 2021). In Alzheimer’s disease, lowering dietary carbohydrates increases brain glucose uptake by 15%, slowing memory decline and offering hope where pharmaceuticals have failed (Cunnane et al., 2016).
Resistance training improves insulin sensitivity by 20–30% within months as muscle mitochondria increase glucose uptake, reversing insulin resistance (Holten et al., 2004).
Intermittent fasting protocols, such as 16:8 or 24-hour fasts, reduce insulin exposure and reverse insulin resistance by 40% in prediabetic individuals within weeks (Sutton et al., 2018). A two-year study on carbohydrate restriction showed that 54% of Type 2 diabetes patients discontinued medication, including insulin therapy, providing strong evidence of near or total reversal (Hallberg et al., 2018).
Call to Action
Insulin resistance represents a critical metabolic threshold, yet current interventions remain misguided. Universal HOMA-IR testing is essential to detect insulin resistance early and prevent chronic disease. Dietary guidelines must shift from a carbohydrate-centric model to one that prioritizes metabolic health through reduced consumption of refined starches and sugars, increased protein and natural fats, and improved sleep and exercise habits.
Dr. Benjamin Bikman, a renowned metabolic scientist and BYU professor with a Ph.D. in Bioenergetics, is the world’s voice of insulin resistance as the root cause of chronic diseases through his groundbreaking research and bestselling book Why We Get Sick.
Article Reference: Insulin Resistance – References





