
Obesity in Adults
Breaking the Obesity Code: How Insulin Dysregulation and Environmental Toxins Collide in a New Disease Paradigm
“Obesity is a chronic, relapsing, multifactorial, neurobehavioral disease, wherein an increase in body fat promotes adipose tissue dysfunction and abnormal fat mass physical forces, resulting in adverse metabolic, biomechanical, and psychosocial health consequences.” Obesity Medicine Association[1]
“For every complex problem there is an answer that is clear, simple, and wrong.” H. L. Mencken
The obesity epidemic is the most pressing public health challenge of our time. Obesity rates continue to rise globally[2] now exceeding 40% in the USA[3]. Obesity costs the US healthcare system almost $173 billion a year [4]. Over 200 diseases are impacted by obesity [5] such as type 2 diabetes, hypertension, cardiovascular disease, sleep apnea, musculoskeletal disease, neurodegenerative diseases, fatty liver, and certain cancers, which can significantly impact overall health and quality and length of life[6] [7] [8]. At a BMI of 40+ your life expectancy is 10 years less which is comparable to smoking[9]. On the world stage the USA is not performing well [10].
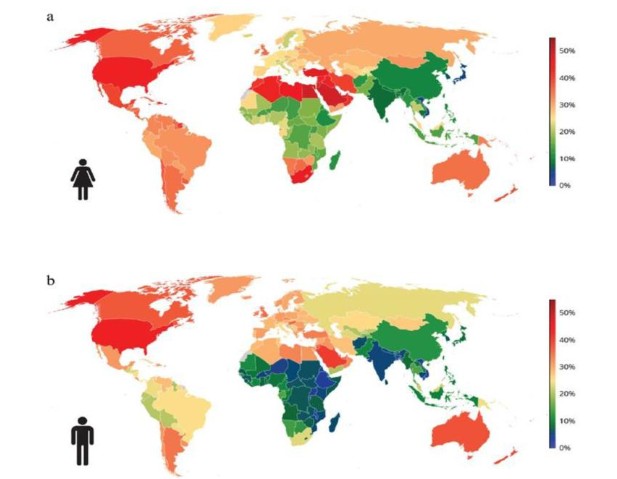
The worldwide prevalence of obesity in 2025: (a) females and (b) males. Obesity refers to BMI ≥ 30 kg/m2. Age-standardized estimates for adults aged 20 years and older. Data obtained from NCD-RisC study. (ref 10)
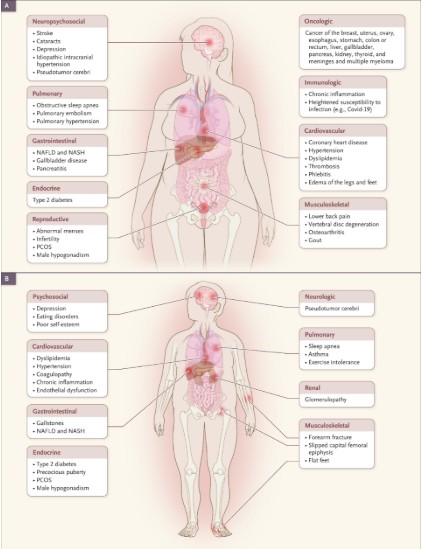
Complications of Obesity in adults (Panel A) and children (Panel B) : N Engl J Med 2022;386:768-779 [11]
A mirror to society at large, obesity in the U.S. military is rising, impacting recruitment, retention, and readiness. In 2002, less than 8% of active-duty service members had obesity[12], increasing to 22% by 2022[13]. This trend threatens national security, with 77% of young adults (17-24) ineligible for military service—36% due to weight[14]. By 2030, 50% of U.S. adults may have obesity, worsening the issue[15]. Obesity also compromises readiness, doubling rates of hypertension, diabetes, sleep apnea, and mental health disorders while increasing injury risk by 33-47%, contributing to over 3.6 million injuries from 2008-2017[16] [17] [18].
Maffetone et al. outlined the real medical issue in their 2016 article Overfat and Underfat: New Terms and Definitions Long Overdue [19]. The term “overfat” is defined as excess adiposity that impairs health. This has been more recently defined as Clinical Obesity by The Lancet [20]. According to Maffetone: “the estimate of this global burden likely exceeds 70% and in certain ethnicities especially Asians there is a large burden of overfat without meeting BMI criteria of obesity. Overfat occurs in overweight, obese, and includes significant numbers of normal-weight non-obese individuals. Many with BMI in the obese range are not overfat and not diseased. As such, the overfat pandemic has created a major global economic burden.”
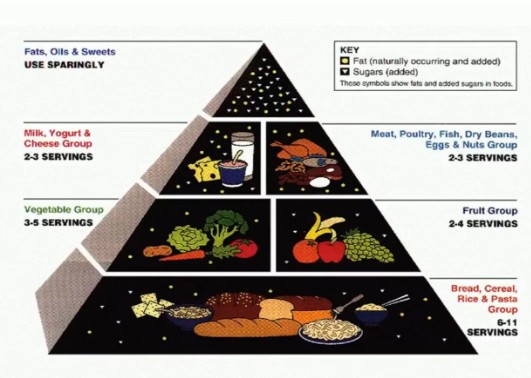
Pyramid Scheme: The Misguided Science Behind Our Obesity Crisis
The 1977 Dietary Goals for the United States aimed to reduce diet-related diseases by lowering fat (30% of daily calories), saturated fat (10%), sugar (under 15%), cholesterol (under 300 mg), and salt intake while increasing complex carbohydrates (55-60% of calories), fiber, fruits, vegetables, and whole grains. These guidelines, particularly the fat and carbohydrate recommendations, sparked controversy and shaped future U.S. dietary policies. The food pyramid originated in Sweden in 1974 [21] as a guide to affordable eating. It was adopted by the U.S. Department of Agriculture (USDA) in 1992 based on these 1977 Dietary Goals and later evolved into “MyPlate” in 2011.
Despite decades of research and interventions focused on the energy balance model (EBM) [22] [23], which considers carbohydrate foods low energy density, there is no flattening the curve of obesity. The EBM has failed to effectively address the global obesity pandemic, as evidenced by the persistent rise in obesity rates despite decades of public health campaigns promoting reduced calorie intake and increased physical activity [24].
Obesity Unstoppable: Time for New Models Grounded in Science and Clinical Insight
Two alternative models have emerged that offer new perspectives on the root causes of obesity: the Carbohydrate-Insulin Model (CIM) proposed by David Ludwig and colleagues [25] [26], and the REDOX/Obesogen Model, recently explored in a 2024 paper co-authored by Dr. Robert Lustig [27]. We will explore these models and how they may provide a more comprehensive understanding of obesity’s complex etiology.
The Carbohydrate-Insulin Model: A Paradigm Shift
The CIM proposes a fundamental shift in how we understand obesity development. Two decades of work of scientific journalist Gary Taubes also makes the historical, clinical, and scientific argument for the CIM in several books [28] [29] [30] [31]. Unlike the EBM, which posits that overeating drives weight gain, the CIM argues for the opposite causal direction:
The process of storing excess fat drives overeating, not the other way around.
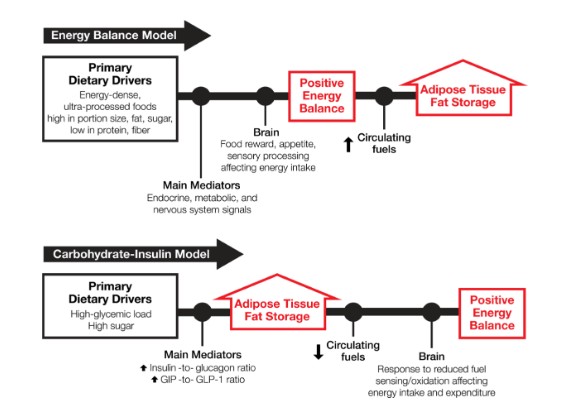
Contrasting causal pathways in obesity models [32]
Key Principles of the CIM
- Hormonal Response to Diet: The CIM focuses on the hormonal effects of different macronutrients, particularly carbohydrates. High-glycemic load diets, rich in rapidly digestible carbohydrates like sugar and processed grains, elicit a pronounced insulin response [33].
- Insulin’s Role in Fat Storage: Insulin acts as a powerful anabolic hormone, promoting the storage of calories in fat tissue while inhibiting the release of fatty acids for energy use [34] [35] [36] [37].
- Energy Partitioning: By directing calories into fat storage, high insulin levels leave fewer metabolic fuels available for other tissues, including the brain and muscles [38] [39].
- Hunger and Metabolic Adaptation: The reduction in available energy triggers biological responses aimed at restoring fuel balance, including increased hunger and appetite, decreased energy expenditure, and fatigue leading to reduced physical activity [40] [41] [42].
- Progressive Weight Gain: Over time, this cycle of energy partitioning and compensatory responses leads to gradual but persistent weight gain [43] [44] [45].
The CIM challenges several core assumptions of obesity treatment:
- Calorie Quality Matters: Not all calories are metabolically equivalent. The hormonal effects of different foods, particularly their impact on insulin, play a crucial role in body weight regulation[46]. Specifically, highly processed food affects appetite regulation [47].
- Limitations of Calorie Restriction: Simply reducing calorie intake without addressing the underlying hormonal drivers of fat storage is likely to be ineffective in the long term [48] [49] [50].
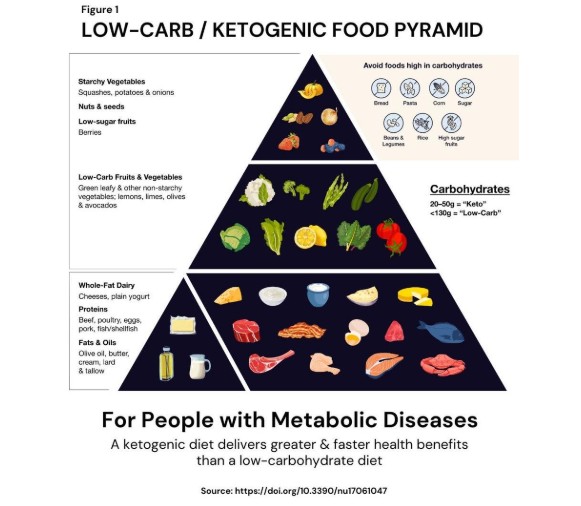
- Focus on Insulin Reduction: Dietary strategies that lower insulin secretion, such as low-glycemic load or ketogenic diets, may be more effective for long-term weight management [51].
- Rethinking Physical Activity: While exercise remains vitally important for health and does facilitate weight loss to a degree, the CIM suggests that increased physical activity alone is unlikely to solve the obesity epidemic if the underlying metabolic drivers are not addressed[52] [53] [54].
The REDOX/Obesogen Model: Environmental Influences on Metabolism
While the CIM focuses primarily on dietary factors, the REDOX/Obesogen Model broadens the scope to include oxidation and environmental chemical exposures as potential contributors to obesity. This model proposes that certain chemicals can disrupt normal metabolic processes and promote weight gain.
Key Concepts of the REDOX/Obesogen Model
- Reactive Oxygen Species (ROS) and REDOX: ROS are naturally produced during metabolism, playing a crucial role in regulating metabolic processes. In small amounts, they function as signaling molecules to maintain balance. However, excessive ROS production—often triggered by overeating, ultra-processed foods [55], or exposure to environmental chemicals—leads to oxidative stress. This imbalance disrupts normal metabolic signaling, increasing insulin secretion, promoting fat storage, and altering appetite regulation, ultimately contributing to metabolic disorders and obesity[56] [57].
- Definition of Obesogens: Obesogens are environmental chemicals that can interfere with various aspects of metabolism, potentially increasing susceptibility to weight gain[58] [59].
- Developmental Origins: The model emphasizes that exposure to obesogens during critical periods of development (in utero, early childhood) may have long-lasting effects on metabolism.
- Epigenetic Effects: Some obesogens may induce epigenetic changes that can be passed onto future generations, potentially explaining some familial patterns of obesity [61].
- Interaction with Diet: The effects of obesogens may be amplified by dietary factors, particularly high-glycemic load diets that promote insulin secretion.
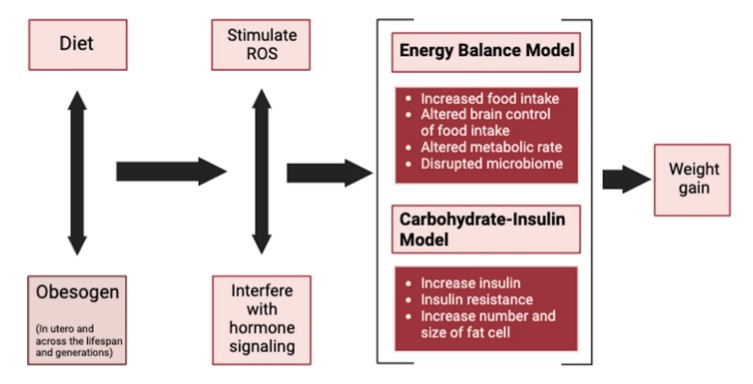
The REDOX/Obesogen model contributes to a unifying theory for the global rise in obesity.
Integrating the CIM and REDOX/Obesogen Model: BOTH/AND
While the CIM and the REDOX/Obesogen Model approach the etiology of obesity from different angles—dietary composition versus environmental chemical exposure—they are not mutually exclusive. Both models shift the focus from individual behavior and highlight the role of external factors in disrupting normal metabolic processes that regulate body weight.
Both hypotheses recognize that hormonal regulation is central to energy balance and fat storage. The CIM focuses on insulin’s role in response to dietary carbohydrates, while the REDOX/Obesogen Model considers how chemicals disrupt hormonal signals related to metabolism and adipogenesis.
There may be interactions between dietary factors and chemical exposures that synergistically increase obesity risk. For example, a diet high in refined carbohydrates could exacerbate the effects of obesogens by further disrupting insulin signaling pathways. Conversely, exposure to obesogens might sensitize individuals to the adverse effects of a high-glycemic diet.
Turning the food pyramid upside down and eating in the manner of the first published low carb pyramid [62] can be part of the solution.
Call to Action
Obesity is a chronic disease driven by genetic, environmental, and hormonal factors—not just lifestyle choices. It disrupts metabolism, increases appetite, and often requires medical treatment beyond diet and exercise. The Carbohydrate-Insulin Model and REDOX/Obesogen Model highlight how hormones and environmental toxins fuel obesity, challenging outdated approaches. To combat this epidemic, we must shift focus to metabolic health, advocate for better treatments, and address environmental contributors. By embracing these insights, we can develop more effective strategies to prevent and treat obesity, improving long-term health for individuals and communities alike.
Dr Mark Cucuzzella is a professor at West Virginia University School of Medicine, is a Metabolic Health Practitioner and board certified in Obesity Medicine.
Article Reference: Obesity in Adults – References





