
Type 2 Diabetes
“Today, one in every nine adults’ lives with type 2 diabetes. Besides increasing the risk for retinal and peripheral nerve complications, diabetes is the most common cause of chronic kidney disease and the strongest risk factor for the leading cause of death in the United States, cardiovascular disease. While some pharmacological treatments have reduced the risk of chronic complications among participants in highly controlled clinical studies, their real-world impact has been much lower in real-world settings. To this day, three interventions have proven to be capable of achieving diabetes remission (defined as not needing medication to sustain normal glucose metrics); gastric bypass surgery, fast-mimicking diets, and ketogenic diets. The real-world effect of the latter is the largest with ~40% of patients achieving remission and all patients achieving better glucose control with less medication”.
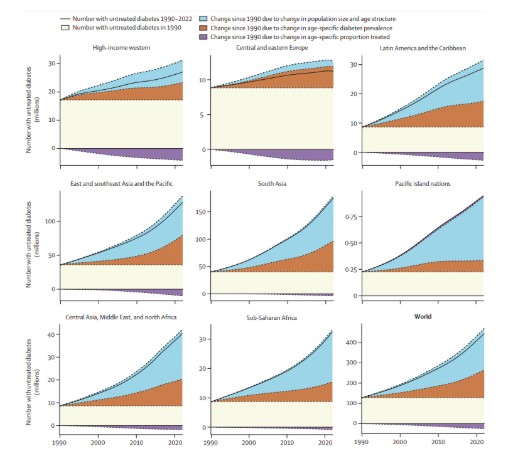
Worldwide, the prevalence and impact of type 2 diabetes mellitus (T2DM) has been rising during the last three decades and, today approximately one in every nine adults live with diabetes. This prevalence increment is observed in all world-regions and is independent of demographic transitions and, alarmingly, is especially large among young adults (Zhou et al., 2024).
It is important to highlight that, while it is frequently perceived as a dichotomous diagnosis, diabetes is, simply, the most severe state in an insulin resistance spectrum in which metabolic and prediabetes are intermediate states.
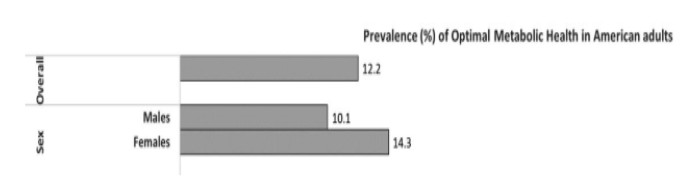
During the last decades, the number and the proportion of Americans with poor metabolic health has increased, and recent studies have shown that more than 88% of Americans present signs of insulin resistance (Araújo et al., 2019).
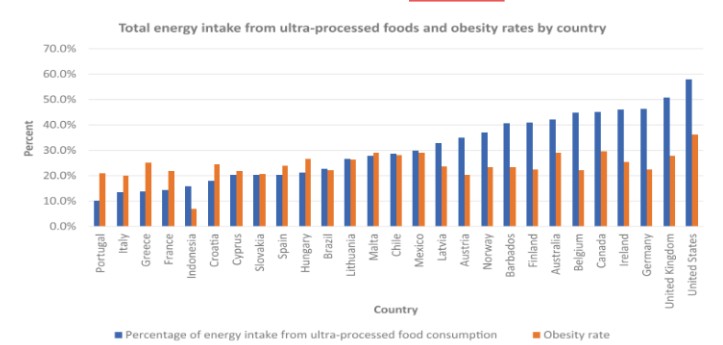
Since population genetic changes cannot account for this prevalence, life-style changes, specifically the simultaneous increment in ultra-processed food consumption is what explains most of this epidemiological change. The United States of America is the country with the largest consumption of ultra-processed foods in the developed world (Crimarco et al., 2022).
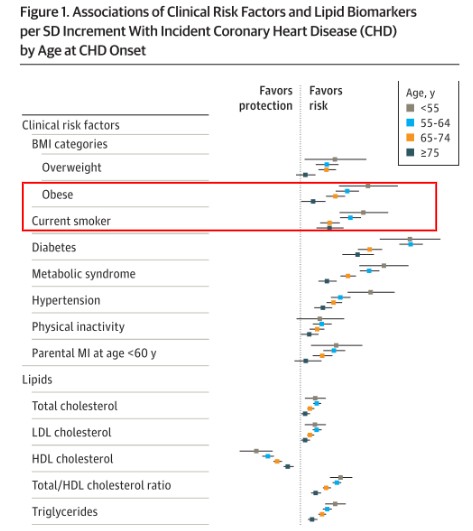
It is worth noting that, in head-to-head comparisons across age groups, insulin resistance (or metabolic syndrome) has a stronger link with CVD than smoking, obesity, hypertension, sedentarism, dyslipidemia, or many other risk factors. Notably, it is the group of young adults in which this risk factor shows its largest magnitude (Mora et al., 2021). In other words, the economic impact of CVD on economically active years in the United States is likely larger than its impact on overall mortality. Nonetheless, it is also important to highlight that T2DM rarely occurs in isolation.
Since it is characterized by insulin resistance, it is not rare that other insulin
resistance associated comorbidities such as obesity, hypertension, dyslipidemia, atherosclerosis, etc. are simultaneously found in people living with T2DM. Consequently, their cardiovascular risk is often worsened by independent and simultaneous mechanisms.
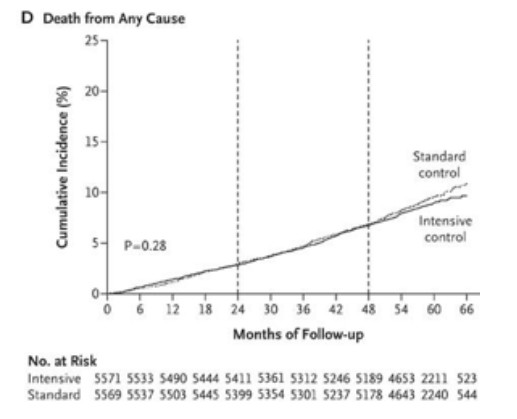
For decades, glucose-lowering drugs achieved micro-vascular complications (i.e., retinopathy, nephropathy and neuropathy) risk-reductions but had no positive impact on macro-vascular ones (i.e., heart attacks, stroke and peripheral artery insufficiency) (Cushman et al., 2010) and their effect on mortality has been documented to be minimal or non-existing (Rodríguez-Gutiérrez & Montori, 2016).
More recently, GLP-1 receptor agonists demonstrated cardiovascular risk reductions in participants enrolled in highly controlled clinical trials (Marso et al., 2016). However, if prescribed for all eligible American citizens, would result in an insurmountable financial burden (Wright et al., 2023). Moreover, their real-world effect (Bellido et al., 2022; Buenaventura-Collazos et al., 2024; Holmes et al., 2021; Mohammedi et al., 2023; Napoli et al., 2023) has been documented to be much lower than what has been documented in the ideal conditions of highly controlled trials (Jastreboff et al., 2022; Wilding et al., 2021).
On the other hand, it is crucial to realize that, in a large proportion of people, T2DM is a reversible state. The American Diabetes Association defines T2DM remission as not needing medication to sustain normal glucose metrics (Riddle et al., 2021).
To this day, no medication has been documented to achieve T2DM remission, and three interventions have proven to be capable of achieving diabetes remission (defined by; gastric bypass surgery, fast-mimicking diets, and ketogenic diets). However, they differ greatly in their therapeutic efficacy, safety and tolerability profiles.
Bypass surgery is the first intervention to document diabetes remission. It did it among people living with severe obesity (which makes it an unviable option for people living with diabetes and normal or close-to-normal weight). It should be noted that patients undergoing these procedures also modify their diet and receive life-style counseling. In fact, it has been observed that most of the physiological changes observed in these patients are already in place before the surgery is performed. The accompanying lifestyle changes are the main driver of these therapeutic interventions (Herzog et al., 2020).
Fast-mimicking diets have also shown to achieve diabetes remission by facilitating liver and pancreatic fat oxidation (Taylor et al., 2019). However, their long-term tolerability is low especially outside highly controlled settings, and its efficacy is comparable to dietary approaches that do not restrict energy intake (Nicholas et al., 2021).
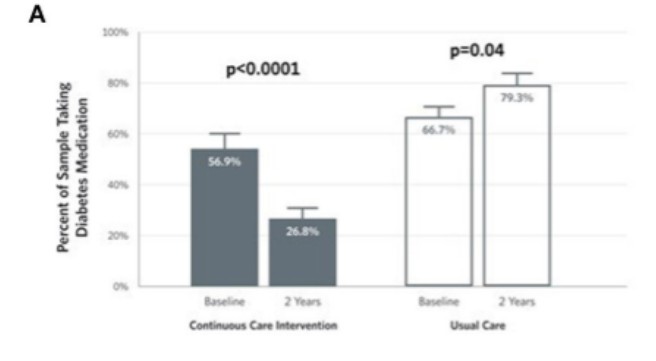
The real-world effect of lifestyle intervention programs based on ketogenic diets has documented that ~40% of patients achieve remission and that all patients achieve better glucose control with less medication” (Athinarayanan et al., 2019; Unwin et al., 2023). Moreover, adherence has been observed to be as high as 80% over one year (Buchanan et al., 2025).
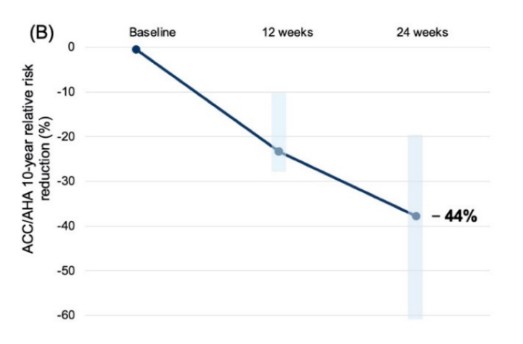
It is also important to highlight that besides improving glucose control, ketogenic diet interventions have demonstrated to reduce cardiovascular risk and to have an even larger therapeutic effect on the frequently found insulin-resistance associated comorbidities than the one observed in dietary interventions specifically developed to treat these comorbidities like the DASH diet, (Saslow et al., 2023).
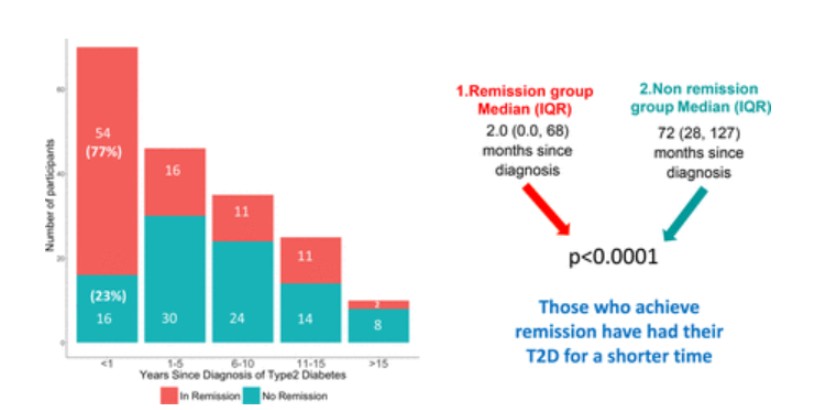
Finally, and emphasizing the importance of screening and prompt implementation, it should be mentioned that there seems to be a crucial therapeutic window to increase the likelihood of achieving diabetes remission. Patients who have lived with diabetes for less than five years and those who have lower glycated hemoglobin levels are more likely to achieve diabetes remission. Nonetheless, most participants can reach their
therapeutic goals with oral medication regardless of their time living with this disease (Unwin et al., 2023).
Call To Action
Diabetes remission is possible, and it starts with the right nutrition and lifestyle choices. By adopting a low-carbohydrate, nutrient-dense diet, prioritizing physical activity, managing stress, and improving sleep, individuals can take control of their metabolic health. Research shows that these interventions can lower blood sugar, reduce medication dependence, and, in many cases, put type 2 diabetes into remission. It’s time to move beyond managing symptoms—let’s empower individuals with the tools to reverse the disease and reclaim their health. The path to remission begins with education, action, and support—start today!
Dr. Adrian Soto-Mota, an MD and Ph.D. from Mexico and Oxford is a leading clinical researcher at the National Institute of Medical Sciences and Nutrition Salvador Zubirán. Dr Soto Moto treats patients with chronic metabolic disease and publishes extensively on metabolic health, nutrition interventions, and evidence-based medicine.






