
Armed Forces
Unfit to Serve: The Metabolic Health Crisis in the U.S. Military
Poor Metabolic Health Impacts Recruitment, Retention, Readiness and Resilience
The United States military, long regarded as one of the most disciplined and physically fit institutions in the world, is facing an unprecedented metabolic health crisis that is making recruits unfit to serve. Obesity rates in the U.S. military have been steadily rising over the past three decades. According to data from the Centers for Disease Control and Prevention (CDC), nearly 20% of active-duty service members were overtly obese in 2020, up from 16% in 2015.
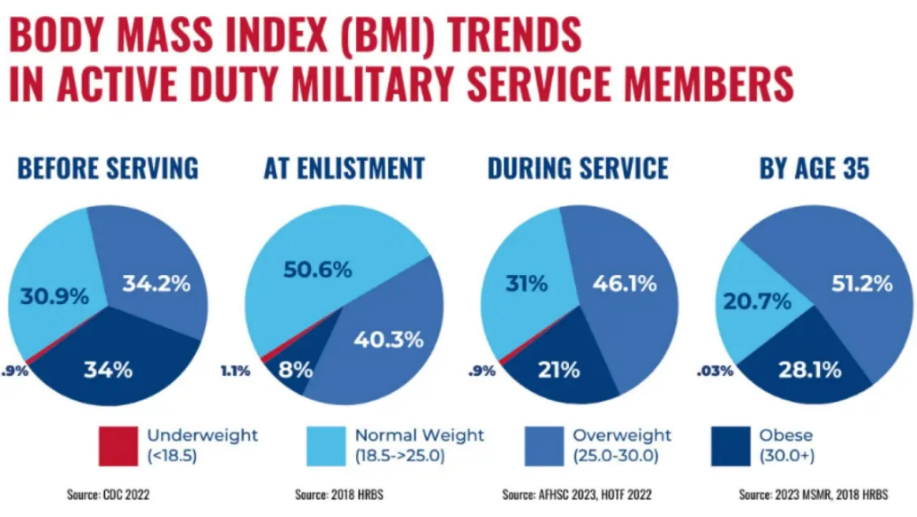
Currently 77% of young Americans (ages 17-24) are now ineligible for military service and obesity is the primary disqualifying factor. Obesity and poor metabolic health in the military represents a national security issue. Additionally, once recruits are in the system, obesity and related comorbidities worsen and contribute to non-deployability and early discharge, further weakening military readiness while increasing health related expenses.
Obesity has wide-ranging implications for healthcare costs. Service members that are obese are at higher risk for musculoskeletal injuries, cardiovascular disease, type 2 diabetes, and mental health disorders. The link between poor metabolic health and mental health disorders is another pressing concern for the military. According to the Department of Defense (DOD), mental health conditions are the leading cause of hospitalization for active-duty personnel. Individuals that are obese or in poor metabolic health are at increased risk of depression, anxiety, post-traumatic stress disorder (PTSD), and substance use disorders. The DOD’s FY2024 budget included a significant investment in mental health services, with $1.4 billion allocated for clinical mental health programs. Initiatives that focus on improving metabolic health will likely have the greatest return on investment for improving these health outcomes.
Causes and Strategies to Improve Military Metabolic Health
The problem of obesity and declining metabolic health in the US military is multifactorial and likely rooted in poor nutrition and dietary patterns, often established in childhood. Poor eating patterns coupled with easy access to nutrient-poor foods and ultra-processed foods high in added sugar and carbohydrates in mess halls, commissaries, and in meals ready to eat (MREs) fuel the problem. In addition, the high-stress of military service can disrupt sleep and result in excess consumption of processed carbohydrates, sugary foods, and sugar-laden energy drinks. Stress and sleep disruption elevates cortisol, and promotes insulin resistance and fat storage. The stress-induced metabolic dysfunction can be largely mitigated by improved nutrition or prescribed dietary interventions.
Historically, the military has focused primarily on “fitness” and physical activity as the main driver to promote weight loss. The prevalence of overweight and underprepared recruits has required the development and implementation of the Future Soldier Prep Course (FSPC) just to meet minimal fitness standards before basic training. Targeted fitness programs aimed at reducing obesity are absolutely essential, but studies have shown that military personnel following a diet low in carbohydrates experienced remarkable improvements in body composition, visceral fat, and glycemic control. In addition, some studies suggest that diets that are very low in carbohydrates can improve endurance and stamina, which are crucial for military performance. Given that daily structured physical activity in the military is mandatory with 24/7 access to on-site-gyms, the same structured discipline, coaching, and access to a well-formulated low carbohydrate diet (or MREs) should be equally prioritized, especially for overweight and obese individuals.
The following 8 guidelines will drastically improve metabolic health:
- Mandate Healthy Food Availability Across All Military Bases: Dining facilities (DFACs) can be restructured to offer healthier options, higher in protein and healthy fat, lower in carbohydrate, nutrition labeling, and meal planning.
- Upgrade MREs (Meals Ready-to-Eat): Current MREs are high in sugar and carbohydrates (>50%) and average only 13% protein. Offer customizable MRE without candy, cookies, or added sugar. Reformulate ALL MREs to include more protein (30%), fiber, and healthy fats.
- Reform Food Contracts & Supply Chains: Prioritize Whole, Unprocessed Foods and Work with suppliers to source fresh, locally grown produce and minimize reliance on ultra-processed meals.
- Reduce Sugary & Processed Foods: Limit the availability of sugar-laden stimulant-filled energy drinks, and processed high-sugar snacks in dining facilities and vending machines. Replace sugary sodas with low or zero sugar beverages, with electrolytes and necessary supplementation.
- Mandatory Nutrition Training for Service Members: Integrate nutrition courses into basic training and ongoing military education. Provide guidance on meal planning, portion control, and performance-enhancing diets and supplementation. Provide access to Registered dietitians (RDs) to assist with meal planning.
- Command Support: Encourage leaders to incentivize and set an example by prioritizing nutrition optimization. Recruits are highly responsive to leadership demands and supportive environments that focus on nutrition as a primary lever for their personal fitness goals.
- Metabolic Monitoring and Feedback: Issue smartwatches, fitness trackers, or continuous glucose monitoring (CGMs) devices to track dietary habits, activity levels, and metabolic markers, especially for obese individuals. Implement routine metabolic screenings (A1C, Trigs, BMI, body fat percentage) and use predictive analytics to identify high-risk individuals and provide early interventions to prevent discharge and enhance readiness.
- Collaboration with Civilian Institutions: Partnerships with academic institutions to develop evidence-based nutritional interventions for metabolic health. Increase the budget for programs like the DOD Congressionally Directed Medical Research Programs (CDMRP) in Nutrition Optimization (NO) to spearhead programs on optimal metabolic health.
Conclusion
The increasing rates of obesity, poor metabolic health, and mental health challenges among U.S. military personnel represent a serious and multifaceted crisis. This not only compromises the individual well-being of service members, but also threatens national security by reducing military readiness and shrinking the pool of eligible recruits. The implementation of dietary reforms coupled with leadership-driven culture change have the greatest potential to reverse these trends. Improving military nutrition requires a multi-pronged approach, including reforms, personalized education, food policy changes, and leveraging technology. Continued investment in these proactive metabolic health strategies will be essential. A metabolically healthy military force is not only stronger, but also physically and mentally more mission-ready, resilient, and will drastically reduce the financial burden.
Dr. Dominic D’Agostino, a tenured Associate Professor at the University of South Florida and Research Scientist at IHMC, is a world leader in metabolic medicine through his groundbreaking research on ketogenic diets and metabolic therapies, demonstrating their potential in treating epilepsy, neurodegenerative diseases, cancer, and enhancing performance in extreme environments.
Article Reference: Armed Forces – References





