Food Product Labeling
Food Product Mislabeling Is Killing Patients – The Deadly Consequences of Misinformation
Introduction
Food labels aren’t just about counting calories or managing weight. They are a matter of life and death for millions of people, particularly those with metabolic disorders like Juvenile Diabetes. While mislabeling contributes to the epidemic of obesity, food addiction, and chronic disease, its most egregious consequence is its potential to kill patients—patients who rely on precise nutritional information to survive.
A recent Congressional hearing with RFK Jr., has reignited the conversation on food transparency and the toxic food environment in America. “…but you should know what the impact of that (food) has on your and your family’s health.” -RFK Jr.
This hearing underscored a fundamental argument:
- Consumers deserve to know what’s in their food—and what it does to their bodies.
This point is acknowledged by the FDA Commissioner of Food and Drugs at the 2024 American Diabetes Association conference when he highlighted the irony that the food products and their labels have contributed to a metabolic health crisis in America that we must now treat this crisis with drugs that cost consumers $10,000-$20,000.

Indeed, today’s food industry with misleading labels, hidden ingredients, and regulatory failures is endangering millions…and NO, I am not talking about obesity. While the conversation around food misinformation has largely focused on obesity and how the modern food environment subconsciously drives overconsumption, it is not the most lethal one. The most devastating failure of food mislabeling, which shockingly no one is speaking about, is its ability to kill vulnerable patients—take children with Juvenile Diabetes—a single fraudulent food label can mean the difference between miscalculating their insulin dose—triggering a deadly blood sugar crash or spike.
The High-Stakes Reality: Case Study- Juvenile Diabetes
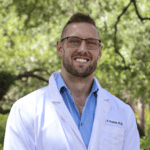
Juvenile Diabetes (T1D) is an autoimmune disease affecting over 8 million people worldwide, with cases expected to double in the next 15 years. Unlike Type 2 Diabetes, T1D is not preventable—it requires lifelong insulin therapy and meticulous glucose control at every meal.

Every Bite is a Calculation
For T1D patients, food is not just nutrition—it’s a dangerous balancing act. They must constantly calculate:
- How many carbohydrates are in this meal?
- How fast will these carbs enter the bloodstream?
- How much insulin should I take to compensate?
Too little insulin? Blood sugar skyrockets, increasing the risk of long-term complications like heart disease, kidney failure, and nerve damage.
Too much insulin? Blood sugar plummets, leading to seizures, loss of consciousness, or even death.
Every. Single. Meal.
And yet, the very food labels these patients rely on to make these life-or-death calculations are often inaccurate, misleading, or downright false.
The Fatal Flaw in Food Labeling
Food manufacturers exploit loopholes in labeling regulations, making it nearly impossible for consumers—even those with medical training—to accurately determine how a product will impact blood sugar levels.
Example 1:
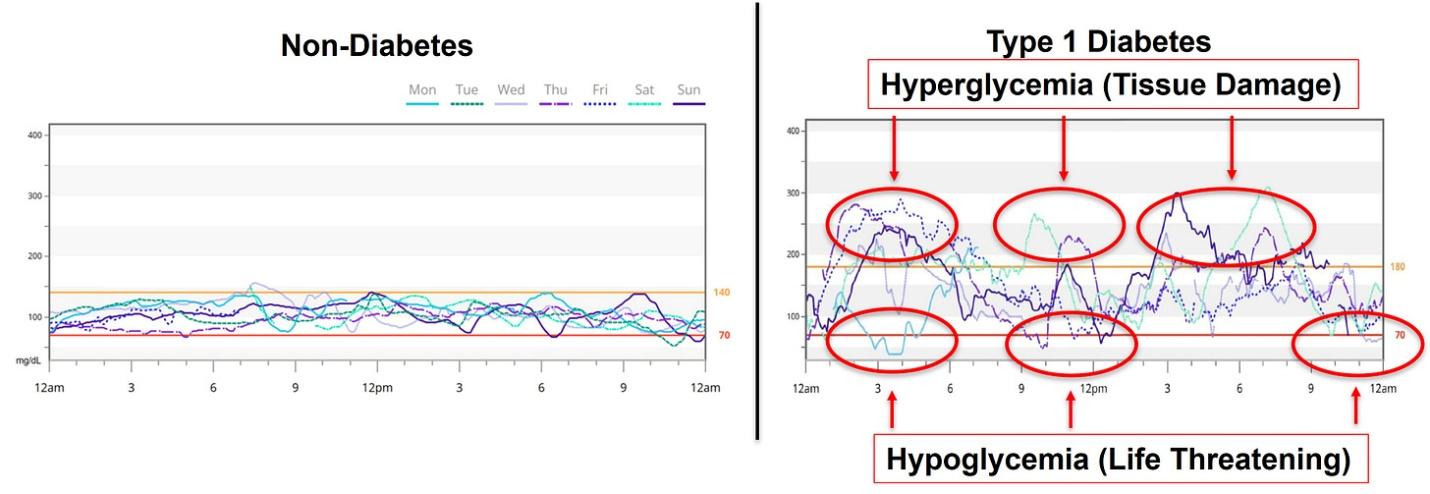
A food product marketed as “keto” or “ketogenic” (low-carb, no blood sugar impact) should, by definition, have little to no effect on glucose levels. Yet, when you scrutinize the actual ingredients list, you often find:
- Hidden sugars disguised under names like maltodextrin, dextrose, or “tapioca fiber.”
- Sugar alcohols that raise glucose levels but aren’t labeled as such.
- “Net Carb” claims that are completely misleading.
There are over 100 different food-label names that allow food companies to not report “sugar” on their label, despite the ingredient being a sugar or having identical or similar metabolic effects as sugar utilizing different naming conventions (sign up at andrewkoutnik.com to receive a complete list of these hidden sugar and sugar replacements) which include:
- Syrups
- Cane Sugar Derivatives & Unrefined Sugars
- Sugar Alcohols, Simple Sugars & Oligosaccharides
- Natural Sweeteners & Plant-Base Sugars
- Whole Grains & Pseudo-Grains
- Processed Grains & Flours
- Starches & Root-Based Flours
A T1D patient relying on this false label would under-dose their insulin, believing the product has little to no carb impact. The result? A dangerous glucose spike of 100–200 mg/dL. Event like this are often commonplace with the current food environment (see picture above) and repeated over time risk of complications, hospitalization, or even diabetic ketoacidosis (DKA), a life-threatening condition.
(Real blood glucose and insulin response of food labeled “Keto Friendly” food product. Product labeling in the United States allowed companies to use “Keto Friendly” and other claims so long as it is not a direct health claim. Look at the CGM and insulin graph when consuming this product. Glucose spiked >200mg/dL with a 300% increase in total insulin requirements immediately afterward.)
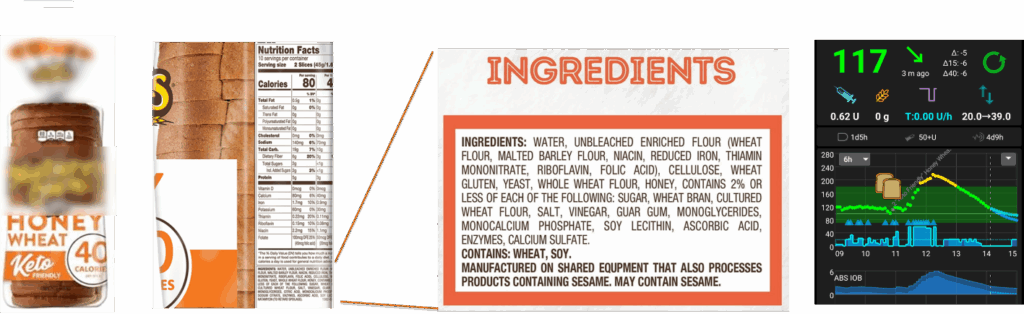
Example 2: Government-Mandated Mislabeling
Some non-glycemic sweeteners—like allulose—have little to no effect on blood sugar levels. But current FDA regulations require these ingredients to be labeled as “carbohydrates”, despite their minimal impact on glucose. This can completely misguide patient to take insulin for carbohydrates on a label, when the ingredients have no carbohydrate-like effect on blood glucose.
For a Type 1 Diabetic, this means they may take insulin for carbs that don’t actually affect blood sugar, leading to a dangerous overdose and a life-threatening hypoglycemic event.
Real blood glucose and insulin response of Allulose-Based Product. Product labeling in the United States requires companies to label ingredients like allulose with no glycemic impact as “carbohydrates” even if they have no blood glucose impact. Look at the CGM and insulin graph. No effect on glucose or insulin immediately afterward.
Both examples have the same calories with nearly identical “Total Carbohydrates” values, but wildly different glucose and insulin impacts. How is a customer supposed to decipher through this? What is the consequence to a patient with Juvenile Diabetes who may overdose on insulin?
The Long-Term Consequences of Food Misinformation
For patients with Juvenile Diabetes, constant blood sugar fluctuations are associated:
- Early vascular dysfunction—starting in childhood (https://pubmed.ncbi.nlm.nih.gov/20097360/).
- Impaired brain development (https://pubmed.ncbi.nlm.nih.gov/24319123/).
- A dramatically shortened lifespan, ranging from 9 to 42 years lost on average (https://pmc.ncbi.nlm.nih.gov/articles/PMC11155716).
- Increased risk for mental health disorders (https://pubmed.ncbi.nlm.nih.gov/29242985/).
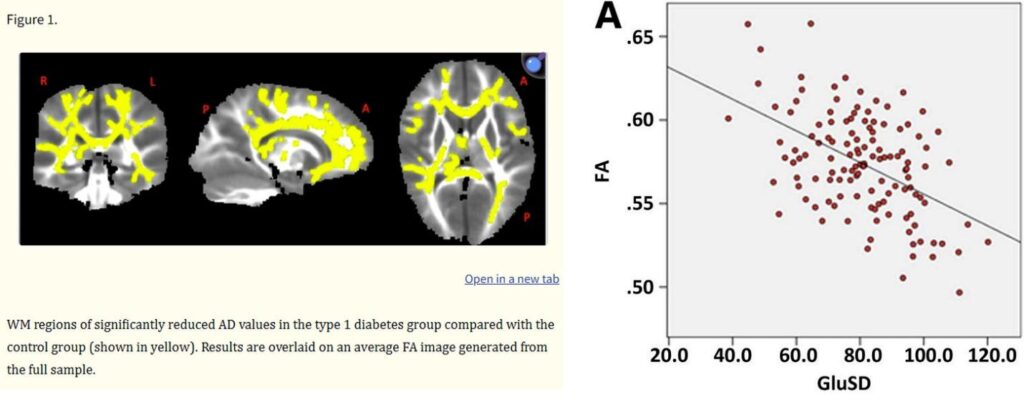
(Data in 4-10year old children (n=127) with Juvenile Diabetes which demonstrated that key areas of brain development are impaired in association with high and variable glucose levels. https://pmc.ncbi.nlm.nih.gov/articles/PMC3898758/)
And this isn’t a patient problem. Patients are often doing everything they are told to control their disease—it’s a systemic failure contributed to by
- Food marketing and misleading labels
- Lack of resources and tools around nutrition
The Urgent Need for Change
Misleading food labels aren’t just about consumer rights—they are about human lives.
- We need to ensure that food labels accurately reflect the metabolic impact of their ingredients.
- We need transparency so patients can make informed decisions without a PhD in metabolism, nutrition, or biomedical sciences.
- We need accountability from both government and private sectors to dramatically reduce the risk patients experience in our current food environment.
Conclusion
The food industry’s misinformation is not just fueling obesity and chronic disease—it’s actively endangering lives. Patients with Juvenile Diabetes do not have the luxury of guessing games when it comes to food. Their survival depends on truthful, accurate food labeling.
And right now, that truth is being hidden. At what cost?
It’s time to demand transparency, accountability, and real change. Lives depend on it.
Andrew Koutnik, PhD, is an award‑winning Research Scientist and globally recognized authority on metabolic health, diabetes management, and human performance optimization, having collaborated with leading institutions.