
Pandemic Preparedness
The Looming Crisis: Metabolic Disease Amplifies Pandemic Vulnerability
“As we reopen society and search for medicines and vaccines that could improve coronavirus outcomes, we should not miss the opportunity to talk about the conditions that have increased our vulnerability to this pandemic in the first place: America’s poor state of health” [1].
The COVID-19 pandemic has had a devastating impact on global health, disproportionately affecting individuals with metabolic health conditions. Among the most significant risk factors for severe outcomes were obesity and metabolic diseases such as type 2 diabetes and metabolic syndrome. We will explore the relationship between these conditions and COVID-19 severity, examining the mechanisms that contribute to increased risk and discuss potential interventions.
Understanding Obesity, Metabolic Disease, And COVID-19: A Deadly Combination
Obesity is defined by excessive adiposity, a body mass index (BMI) of 30 kg/m² or higher. When the excessive adiposity is in the visceral spaces and ectopic spaces (around and in organs themselves as well as intramuscular fat) the terrain is fertile for infection and inflammation [3][4]. This is what the current Lancet Commission describes as “Clinical Obesity” [5].
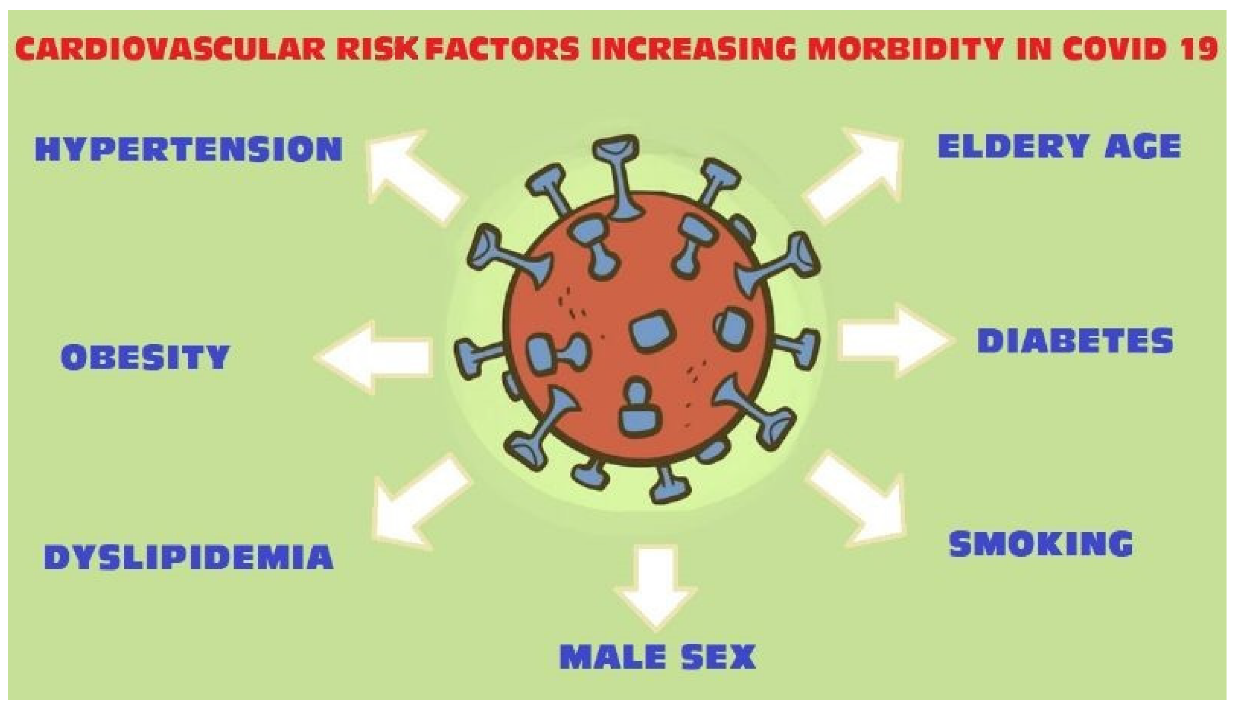
Clinical Obesity is synonymous with metabolic diseases, including insulin resistance, type 2 diabetes, hypertension, CVD, and dyslipidemia [6] [7]. These conditions collectively contribute to metabolic syndrome, a cluster of abnormalities driven by the high insulin state [8] that significantly increase cardiovascular risk, neurodegenerative diseases, many cancers, and the spectrum of type 2 diabetes and its complications.
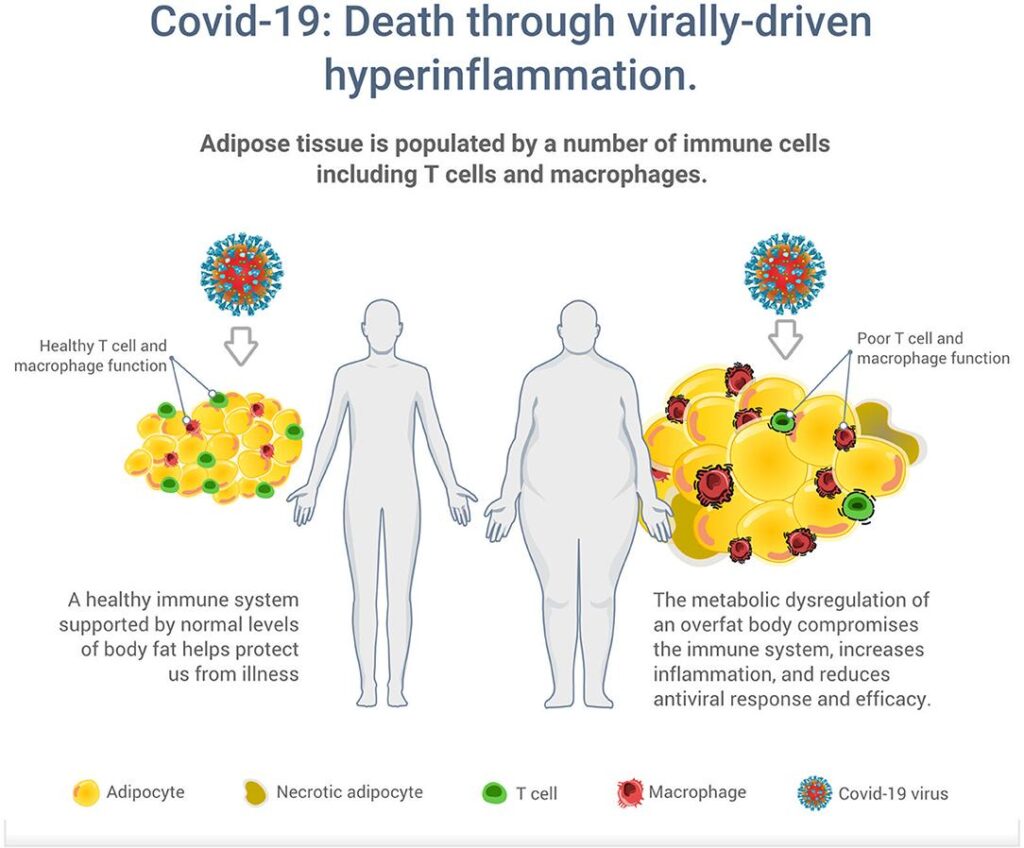
Metabolic disease creates chronic low-grade inflammation [9] [10], predisposing individuals to chronic illnesses and impaired immune function, making them more susceptible to severe infections, including COVID-19. Improved nutrition is a path to reversal [11].
Mechanisms of Multisystem Dysfunction and Increased Risk
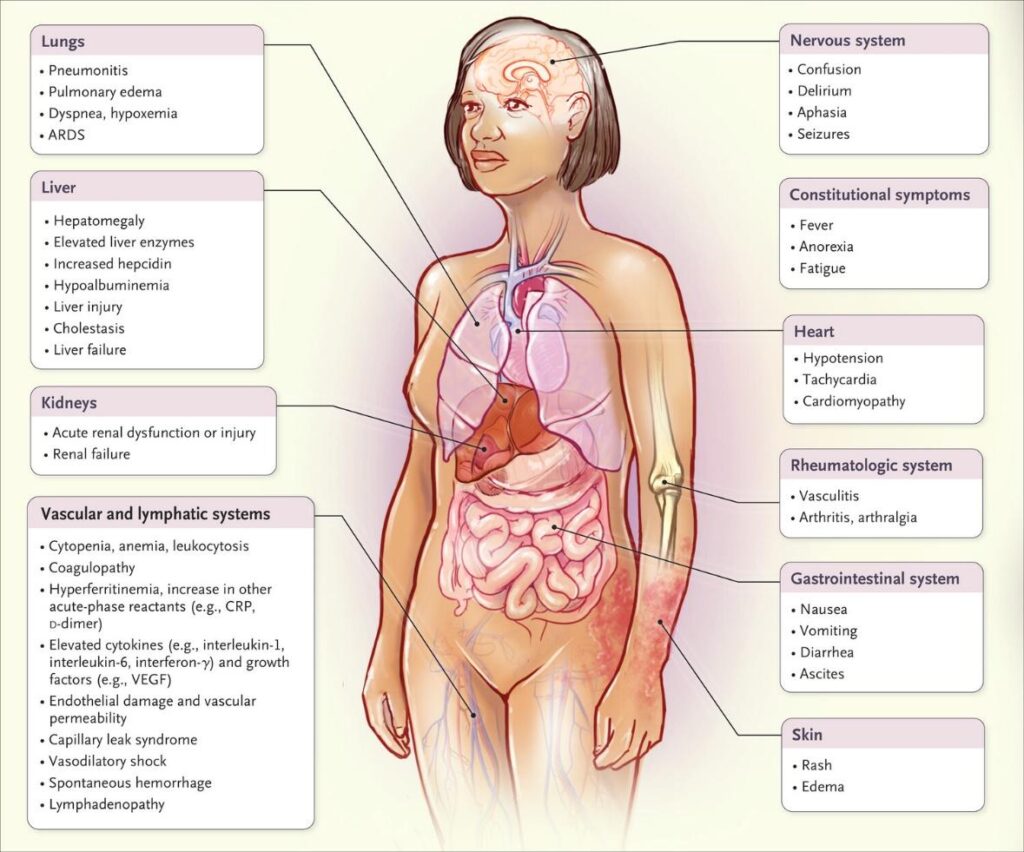
Multiple studies have demonstrated that obesity and metabolic syndrome are independent risk factors for severe COVID-19 [13] [14] [15] [16]. Individuals with obesity are more likely to experience severe symptoms, require hospitalization, and suffer from complications such as acute respiratory distress syndrome (ARDS) [17] and multi-organ failure. The mechanisms driving this increased risk include:
- Impaired Immune Response: Obesity is associated with chronic systemic inflammation and immune dysregulation. Elevated levels of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), contribute to an exaggerated inflammatory response, known as the “cytokine storm,” which is a major contributor to severe COVID-19.
- Respiratory Dysfunction: Excess adiposity can lead to restrictive lung disease, reduced lung compliance, and impaired diaphragmatic function. These factors make it more difficult for obese individuals to compensate for the respiratory distress caused by COVID-19, increasing the likelihood of intubation and mechanical ventilation.
- Increased Risk of Thrombosis: Obesity and metabolic disease are associated with a hypercoagulable state, characterized by elevated levels of clotting factors and endothelial dysfunction [18]. This predisposes individuals to thrombotic complications such as pulmonary embolism.
- Altered ACE2 Expression: Angiotensin-converting enzyme 2 (ACE2) is the primary entry receptor for SARS-CoV-2. Adipose tissue expresses high levels of ACE2, potentially serving as a reservoir for the virus. This may contribute to prolonged viral shedding and increased viral load in obese individuals.
Metabolic Disease and COVID-19 Severity
Beyond obesity, metabolic diseases such as type 2 diabetes significantly increase the risk of severe COVID-19 [20] [21]. Individuals with diabetes are more likely to experience poor outcomes due to the following factors:
- Hyperglycemia and Immune Dysfunction: Elevated blood glucose levels impair neutrophil function, reduce T-cell response, and promote excessive inflammation. This weakens the body’s ability to fight off viral infections, leading to a higher likelihood of severe disease progression.
- Inflammation and Cytokine Storm: Metabolic syndrome is characterized by chronic low-grade inflammation, which can exacerbate the inflammatory response seen in severe COVID-19 cases. This increases the risk of ARDS, multi-organ failure, and death.
- Endothelial Dysfunction and Cardiovascular Complications: Diabetes and hypertension contribute to endothelial dysfunction, making blood vessels more prone to damage. This can lead to complications such as stroke, myocardial infarction, and kidney injury in COVID-19 patients [22].
- Mortality: Obesity has been strongly associated with increased mortality in COVID-19 patients [23].
Misguided Policies and Programs
- Social Distancing and Mask Mandates: The 6-foot distancing rule was later admitted by officials to be arbitrary, lacking scientific basis, and disproportionately harmed schools and small businesses [24] [25]. Mask policies faced criticism for inconsistent messaging, with officials flip-flopping on efficacy without transparent data, eroding public trust [26].
- Vaccine Mandates: Mandates for COVID-19 vaccines were implemented despite limited evidence supporting their necessity for healthy individuals and those with natural immunity. Critics argued these policies disregarded medical freedom, harmed military readiness, and exacerbated distrust in public health institutions [27].
- Neglect of Natural Immunity: Public health agencies systematically ignored natural immunity from prior infection when crafting vaccine guidelines [28].
- Vaccine Injury Systems: Compensation programs for vaccine-related injuries were plagued by inefficiency, opacity, and poor communication, failing to address concerns about rare adverse events and deepening mistrust [29].
- Economic Lockdowns: Broad business closures lacked nuanced risk assessment, causing over 160,000 permanent closures in the U.S. alone [30].
- School Lockdowns: School lockdowns during COVID-19 had significant effects on education, mental health, and social development [31] [32] [33]. Learning loss was widespread with disadvantaged students experiencing the greatest setbacks. Mental health issues among children and adolescents increased due to isolation and lack of routine. Social skills and emotional development were also impacted, as students missed critical peer interactions [34]. While remote learning helped maintain continuity, it often lacked effectiveness due to unequal access to technology and varying levels of engagement [35] [36]. The long-term consequences of these disruptions continue to be studied.
These missteps highlight the challenges of balancing rapid response with scientific rigor during a crisis. We need adaptive, evidence-based frameworks in future pandemics.
Pandemic-Proofing Humanity: Revolutionizing Health Through Diet, Lifestyle, and Metabolic Optimization
A range of nutritional, lifestyle, and metabolic approaches have been explored to reduce the disease burden of COVID-19 by supporting immune function, improving metabolic health, and reducing inflammation [37] [38] [39]. These approaches play an important role in improving outcomes and resilience against the virus [40]. Given the clear link between obesity, metabolic disease, and COVID-19 severity, targeted interventions are crucial [41] [42]. The following strategies can help mitigate risk:
- Reducing the burden of obesity and metabolic disease especially in children: Public health as well as medical prioritization to prevent and reverse these conditions will improve the metabolic health of the nation and reduce infectious disease risk and burden. A diet rich in unprocessed natural food rich in protein, healthy fats, and non-starchy vegetables can support weight loss and reduce inflammation [43] [44] [45]. Regular physical activity enhances insulin sensitivity, reduces visceral fat, and strengthens the immune system [46] [47] [48].
- Prioritize better glycemic control and diabetes remission: Ketogenic or Low-Carb Diets may improve blood sugar control and metabolic flexibility, which are critical for those at risk of severe infection[49] [50]. Better glycemic control is essential to reduce complications in diabetic patients. We must prioritize cost effective medications, consideration of continuous glucose monitoring, and support for lifestyle changes.
- Sleep Optimization, Stress Reduction, Sunlight and Outdoor Exposure: emerging evidence suggests that poor sleep [51] [52] and constant stress [53] [54] weaken the immune system and increase susceptibility to infections. The benefits of sunlight and outdoors is also multifactorial from vitamin D production to direct mitochondrial enhancement [55] [56].
Call to Action
The reality is that we are partially responsible for our fragility to the coronavirus and the pandemic revealed how truly vulnerable we are. We have often blamed the victim for having obesity or other diet-related diseases, but these illnesses now affect up to 80% of the world’s population. Our Covid-19 approach focused on hiding from the virus and immunization to set us free. We believe the best idea going forward instead is to strengthen our resistance to Covid and future viruses, with a healthy immune system—which means a healthy lifestyle.
Reducing sugar, refined carbohydrates, and ultra-processed foods which together fuel insulin resistance, is an ideal first step. Eating to keep blood sugar low and stable will reduce risk. Anyone can purchase a continuous glucose monitor to know exactly how foods are affecting blood sugar levels. Junk food became a quarantiner’s best friend. Yet even these comforting foods can be resisted when replaced by whole, natural foods including natural fats and proteins. It is also critical to focus the diet on foods that are nutrient dense: meats, eggs, seafood, dairy, vegetables, and low-sugar fruits.
Each comorbidity you have decreases your physiological reserve. We should be doing a better job in maintaining our health for times when we are under stress. We hope to see a new world where people have the tools to recover their good health and become stronger to fight pandemics such as Covid. Even as the coronavirus abates, the ongoing obesity, diabetes, and metabolic disease pandemics will continue to take their toll on our society. It is time to take back our health, our own resilience—and that of our nation.
Dr. Mark Cucuzzella, a board-certified family physician and professor at West Virginia University, was at the forefront of the COVID-19 pandemic, illuminating the critical link between metabolic health and COVID outcomes, advocating for lifestyle interventions to bolster resilience against future health crises
* the author worked in a small critical care access hospital in West Virginia during the pandemic
Article Reference: Pandemic Preparedness – References





