
Primary Care
Rebuilding Primary Care: The Cornerstone of Metabolic Health
Introduction
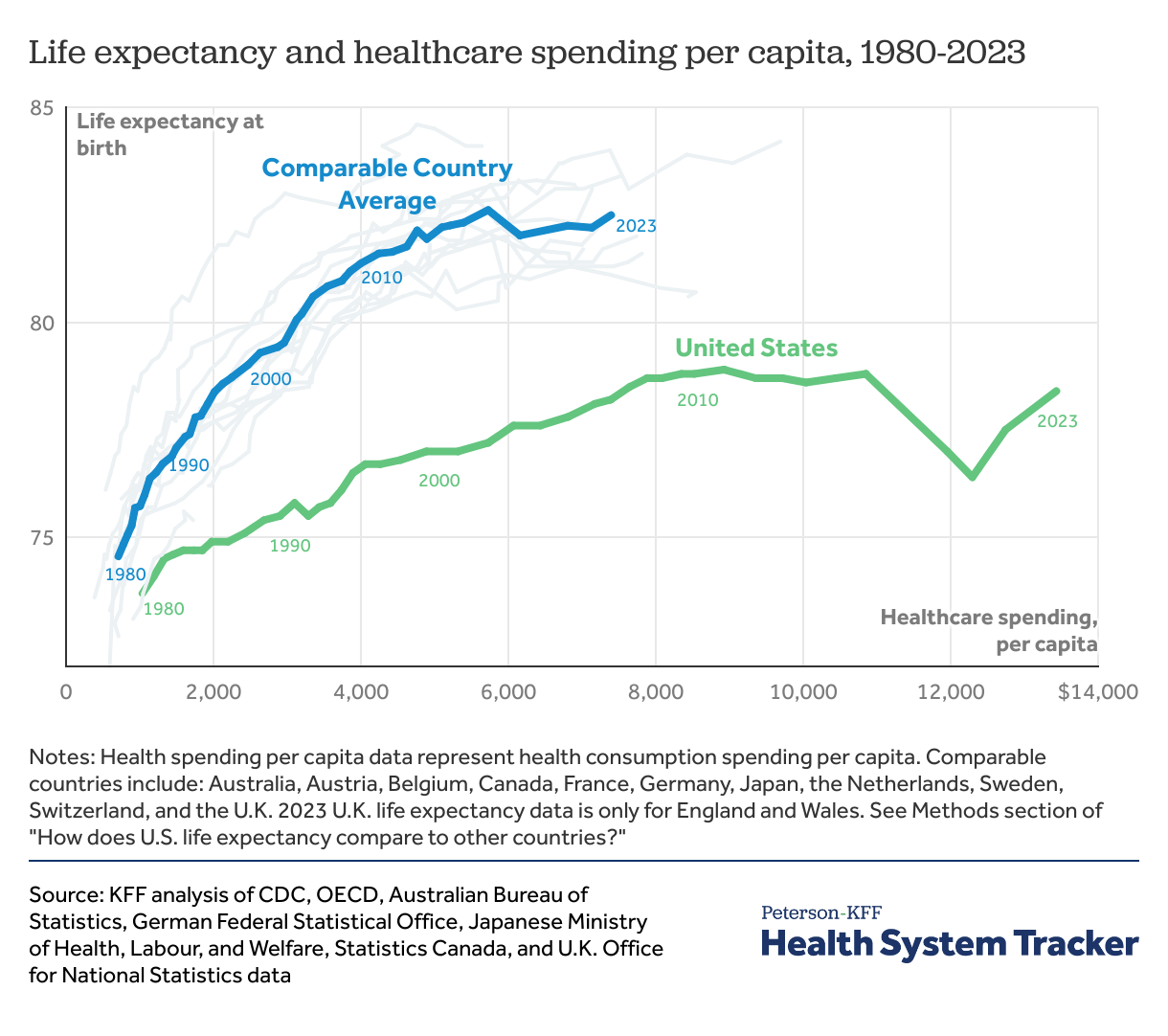
The U.S. healthcare system is the most expensive in the world, yet it consistently lags other developed nations in health outcomes [1]. This failure stems from a system that prioritizes disease management over prevention, leaving a population burdened by chronic illness. To achieve a cost-effective, high-performing healthcare system, we must shift our focus toward strengthening primary care. By equipping clinicians with expertise in metabolic health, we can not only drive down healthcare costs but also prevent chronic diseases, improve patient outcomes, and enhance overall well-being, ultimately transforming the nation’s health.[2] [3]
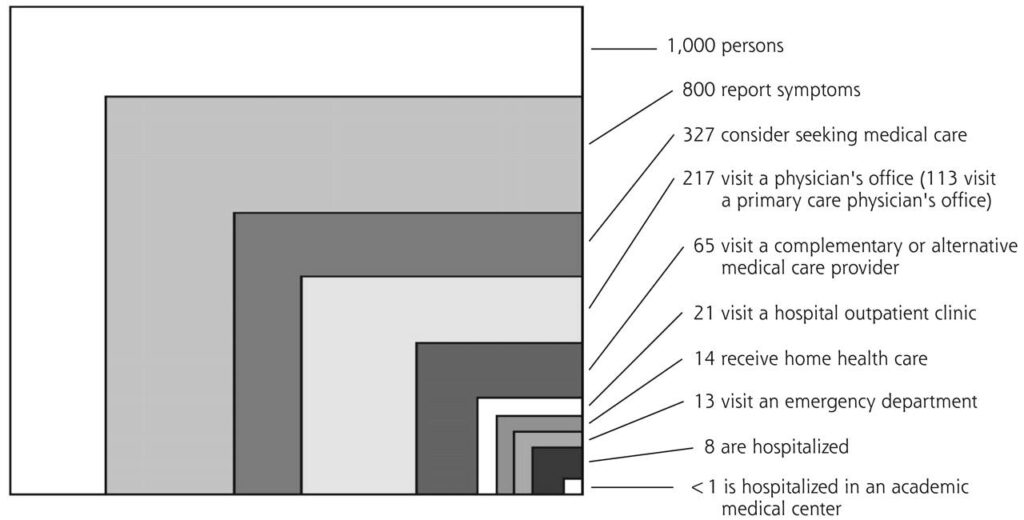
Dr. Larry Green, my former Chair at the University of Colorado, aptly described the vital role of primary care in our healthcare system. While we train physicians in academic medical centers, most patients seek care from primary care providers within their own communities.
The Current State of Healthcare: A Reactive Model
The prevailing model of healthcare in the U.S. is largely reactive, emphasizing specialist care and expensive interventions for treating diseases rather than preventing them [6] [7] [8]. Chronic conditions like diabetes, obesity, and cardiovascular disease drive up costs while being poorly managed within this system [9] [10] [11] [12]. Instead of addressing the root causes—such as poor nutrition, lack of exercise, and socioeconomic disparities—our healthcare system tends to treat symptoms with medications and procedures that provide short-term relief but no lasting solutions [13].
This reactive approach has led to skyrocketing healthcare expenditures, with over 90% of healthcare dollars spent on treating chronic conditions [14] [15]. Meanwhile, primary care—which should serve as the frontline defense against these conditions—remains underfunded and underutilized [16] [17] [18] [19] [20].
The Quadruple Aim of Healthcare must be our goal [21] [22]. It expands on the Triple Aim by adding provider well-being as a key focus with primary care doctors as the foundation. It seeks to enhance patient experience, improve population health, reduce healthcare costs, and support healthcare professionals by addressing burnout and workplace challenges. By prioritizing both patient-centered care and provider well-being, the Quadruple Aim promotes a more sustainable, efficient, and effective healthcare system[23].
Optimizing Primary Care: The Key to a Cost-Effective, High-Impact Healthcare System
Primary care is the foundation of an effective healthcare system because it provides comprehensive, continuous, and preventive care. Countries with strong primary care systems, such as the Netherlands [24] and Denmark [25] [26], consistently report better health outcomes at lower costs. By emphasizing early intervention and holistic patient management, a well-trained primary care workforce can prevent or delay the onset of costly chronic diseases and reduce hospital admissions [27] [28] [29].
Primary care is affordable, improves public health, and can transform the U.S. healthcare system by prioritizing people over profit and addressing inefficiencies. Providing everyone with access to a Primary care doctor will ensure millions receive essential care and enhance the quality for those who already have it[30].
Key benefits of a strong primary care system with expertise in metabolic health include:
- Improved Access to Care: Primary care physicians (PCPs) serve as the first point of contact, ensuring patients receive timely medical attention before conditions worsen.
- Lower Healthcare Costs: Preventive care especially with chronic disease reduces emergency room visits, hospitalizations, and expensive specialist treatments [31] [32].
- Better Chronic Disease Management: PCPs help patients manage diabetes, hypertension, and other chronic conditions through lifestyle interventions and early treatment [33] [34] .
- Enhanced Patient Outcomes: Studies show that patients with access to strong primary care have lower mortality rates and higher life expectancy [35] [36] [37] [38].
- Greater Health Equity: A strong primary care network ensures that underserved populations receive quality care, reducing health disparities [39] [40].
The Barriers to Effective Primary Care
Despite its proven benefits, primary care in the U.S. faces numerous challenges that limit its effectiveness:
- Underfunding and Low Reimbursement Rates: Primary care physicians are among the lowest-paid professionals in medicine due to lower reimbursement rates compared to specialists. This financial disparity discourages medical students from pursuing careers in primary care, leading to a workforce shortage [41]. The trend continued in 2025 [42].
- Physician Burnout and Workforce Shortages: PCPs often face overwhelming patient loads, administrative burdens, and long working hours, leading to burnout and early retirement. The shortage of primary care providers further exacerbates access issues, particularly in rural and underserved areas.[43]
- Fragmented Care Delivery: The healthcare system is structured around specialty care rather than integrated, team-based primary care. As a result, patients receive disjointed care, increasing the risk of misdiagnosis, overtreatment, and unnecessary procedures.
- Lack of Preventive Focus: Due to time constraints and high patient volumes, PCPs struggle to prioritize preventive care and lifestyle counseling. Instead, the system incentivizes quick fixes, such as prescribing medications, rather than addressing underlying lifestyle factors.
- Insurance and Bureaucratic Barriers: The complexity of insurance billing, prior authorizations, and administrative requirements limits the ability of PCPs to spend quality time with patients. These inefficiencies reduce the effectiveness of primary care and frustrate both providers and patients.
- Barriers to Obesity Care: The 2025 Obesity Management in Primary Care: A Joint Clinical Perspective and Expert Review by OMA and ACOFP is an educational resource combining current medical science and clinical expertise. It aims to enhance the care and management of patients with obesity in primary care settings[44].

Strategies for Rebuilding Primary Care
To transition toward a cost-effective, health-focused system, we must prioritize rebuilding primary care through the following strategies:
- Increase Investment in Primary Care: Redirecting healthcare spending toward primary care can lead to significant cost savings in the long run. Policymakers must advocate for increased reimbursement rates for primary care services, ensuring that PCPs are adequately compensated for their essential role in healthcare [45] [46] [47].
- Expand the Primary Care Workforce: To address workforce shortages, medical education must incentivize careers in primary care by expanding loan forgiveness programs for medical students, increasing residency slots for family and general internal medicine, and enhancing mentorship and training programs for future PCPs.
- Implement Team-Based Care Models: Team-based care models, such as the Patient-Centered Medical Home (PCMH), enhance care coordination by integrating physicians, nurse practitioners, dietitians skilled in metabolic health, and mental health professionals. This model reduces physician burnout, improves patient care, and fosters a more holistic approach to health management [48] [49].
- Shift Toward Value-Based Care: The current fee-for-service model rewards volume over quality, leading to unnecessary tests and procedures. Transitioning to a value-based care system aligned with the Quadruple Aim would incentivize PCPs to focus on patient outcomes rather than the number of services provided.
- Strengthen Preventive Care Initiatives: Primary care should prioritize metabolic health by expanding access to lifestyle medicine programs that promote nutrition, exercise, and stress management, increasing screening and early intervention for chronic diseases, and integrating social determinants of health into patient care to address factors like housing, food security, and mental well-being [50] [51] [52].
- Improve medical education with a focus on metabolic health as foundation: Medical schools provide minimal training in metabolic health, leaving many physicians ill-equipped to address conditions like obesity, diabetes, and insulin resistance effectively. The curriculum often prioritizes pharmacologic management over lifestyle interventions such as nutrition, exercise, and metabolic flexibility. A 2019 study in The Lancet [53] found that fewer than 20% of medical schools offer adequate education in nutrition, despite its critical role in preventing and managing chronic disease. Without a stronger emphasis on metabolic health, physicians are left treating symptoms rather than addressing root causes, perpetuating the cycle of chronic illness. [54].
- Reduce Administrative Burdens: Simplifying insurance processes and reducing paperwork can free up more time for patient care. Policymakers must work toward minimizing bureaucratic barriers, improving electronic health records (EHR) usability, and streamlining prior authorization processes [55].
- Embracing Technology and Telemedicine: Telemedicine has the potential to expand primary care access, particularly in rural and underserved communities. By leveraging virtual visits, remote monitoring, and digital health tools, PCPs can provide timely interventions while reducing the need for in-person consultations.
Call to Action
Rebuilding primary care is essential for transforming the U.S. healthcare system from a disease-treatment model to one centered on health promotion, cost-effective care, and restoring metabolic health. By investing in primary care, expanding an educated workforce, integrating preventive strategies, and shifting toward value-based care, we can create a system that prioritizes long-term health over short-term disease management. The time for action is now—strengthening primary care is not just a policy option; it is a necessary step toward a healthier, more equitable, and financially sustainable healthcare future.

Dr Mark Cucuzzella, Fellow American Academy of Family Practice, is a primary care doctor who has helped create culinary programs for medical students [56], implemented low carbohydrate diets in hospital menus [57], and eliminated sugar drinks from a small hospital [58].
Article Reference: Primary Care – References





